Translate this page into:
Philadelphia-positive precursor B-cell acute lymphoblastic leukemia in elderly alcoholic patient – A case report

*Corresponding author: Dr. Gunjan Bala, Department of Pathology, Adesh Institute of Medical Sciences and Research, Bathinda, Punjab, India. 30.gunjan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Suri V, Bala G, Gupta R, Narang S, Gupta A, Bansal N. Philadelphia-positive precursor B-cell acute lymphoblastic leukemia in elderly alcoholic patient – A case report. Adesh Univ J Med Sci Res 2019;1(1):31-3.
Abstract
Philadelphia chromosome is well-known chromosomal abnormality in chronic myeloid leukemia (CML). However, B-acute lymphoblastic leukemia (B-ALL) with Philadelphia-positive (Ph′) is a neoplasm of lymphoblast committed to the B-cell lineage. The clinical presentation of B-ALL Ph′+ is similar to B-ALL but is more common in adults than in children. Our 50-year-old male patient presented to psychiatry OPD for deaddiction of alcohol. The patient also complained of generalized weakness and pain in legs which may have been due to chronic alcoholism. He was further investigated and diagnosed as B-precursor ALL with positive BCR-ABL fusion gene. Here, we like to emphasize that overlapping symptoms may lead to delay in diagnosis, so clinician should always investigate the patient thoroughly so that the patient is diagnosed on time and treatment can be started as early as possible and fatal outcomes can be avoided.
Keywords
Philadelphia positive
Acute lymphoblastic leukemia and elderly male
INTRODUCTION
Acute lymphoblastic leukemia (ALL) is a neoplastic disease of immature lymphocytes or lymphocyte progenitor cells of either the B- or T-cell lineage. Leukemia is the most common childhood cancer in India with relative proportion varying between 25 and 40%. About 60– 85% of all leukemias are reported as ALL.[1] B-ALL with Philadelphia chromosome (Ph′) is a neoplasm of lymphoblast committed to the B-cell lineage. Philadelphia chromosome-positive (Ph1) ALL is defined by the t(9; 22) (q34; q11) translocation that produces BCR-ABL1, a constitutively active tyrosine kinase. BCR-ABL1 fusion is present in essentially all cases of chronic myeloid leukemia and in 3–5% of pediatric ALL and 25% of adult ALL.[2,3] Before the advent of tyrosine kinase inhibitor (TKI) therapy, Ph1 ALL was associated with very poor survival, which has been improved significantly by the early addition of imatinib or related TKIs to intensive chemotherapy regimens with or without hematopoietic stem cell transplantation in the first complete remission.[3-7] The aim of this article is to report a very unusual presentation of a case of ALL in a chronic alcoholic elderly male who visited psychiatry OPD for deaddiction.
CASE REPORT
A 50-year-old male from Northwest part of (Punjab) India presented with complaints of generalized weakness, myalgia, dyspnea on exertion, and loss of appetite for ½ months. The patient was a known chronic alcoholic for 20 years and was on treatment for same for 6 months comprising lorazepam 4 mg HS and thiamine 100 mg BD. His hematological and biochemical investigations were normal at that time apart from hemoglobin which was on lower side, i.e., 9 g.
All the relevant hematological and biochemical investigations were again done on current visit and results were as follows:
Hemoglobin: 6 g%
Total leukocyte count: 7100/cumm
Differential leukocyte: N-10, L-42, B-1, blasts – 46%, and myelocyte – 1%
Platelets: 34,000
Bone marrow aspiration showed hypercellular smear comprising 90% blasts showing anisocytosis with size 1.5–4 times the size of mature lymphocyte with high N:C ratio, round to indented nuclear membrane, opened up chromatin with 1–3 conspicuous nucleoli, and moderate agranular cytoplasm.
No Auer rods were seen.
On light microscopy examination, provisional diagnosis of acute leukemia/lymphoma was made. The patient was advised flow cytometry and molecular work-up to confirm diagnosis and categorization. The patient was referred to PGI, Chandigarh.
Figure 1 Giemsa stained bone marrow aspiration smear showing predominately blasts admixed with few lymphocytes in the background of red blood cells.

- Bone marrow aspiration smear.
Myeloperoxidase stain – negative
Periodic acid–Schiff stain – negative
Pearls stain – 3+
Bone marrow trephine biopsy showed 100% cellularity with sheets of blast cells as described above.
Flow cytometry done at PGI, Chandigarh [Figure 2].
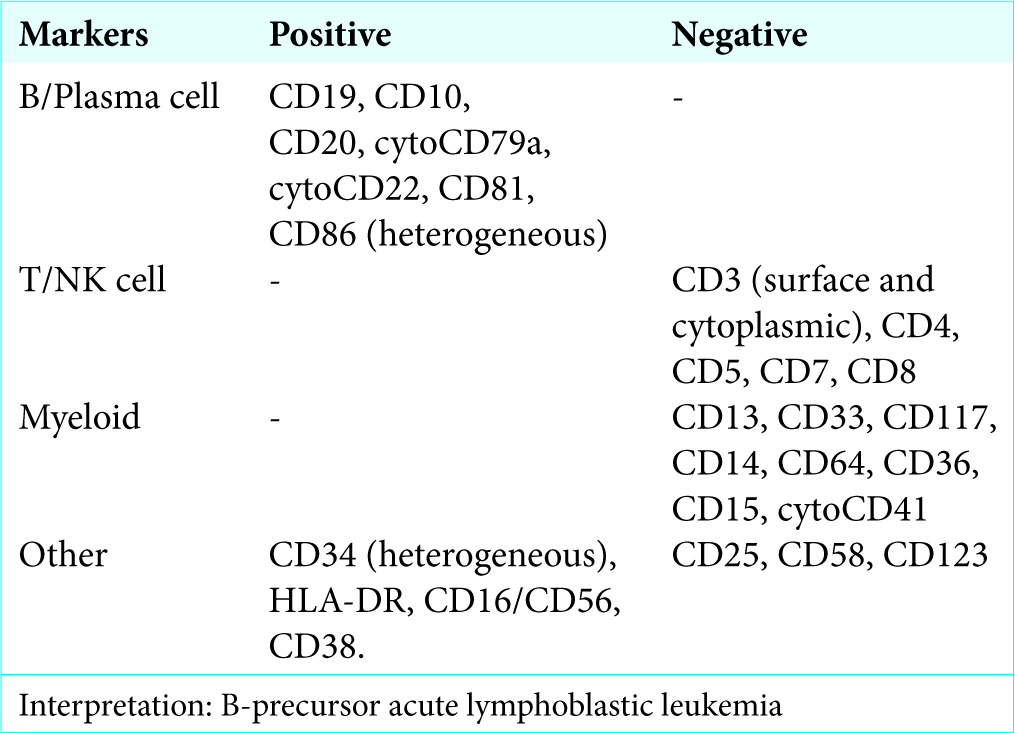
- Flow cytometry report.
Molecular genetic analysis report was done at PGI, Chandigarh Figure 3.

- Molecular genetic analysis report.
RT-PCR for the t(9, 22); BCR-ABL fusion genes are positive.
Ultrasound whole abdomen showed splenomegaly and cholecystitis. He had high random blood sugar (173 mg/dl) and serum uric acid (8.7 mg/dl) and urea (79 mg/dl). All other investigations including liver function test, serum electrolytes, serum protein, and creatinine were with in normal limits. Patients had no significant family history. On clinical examination, the patient was well oriented, afebrile, and normotensive; no lymphadenopathy/ hepatomegaly noted. The patient was diagnosed as BCR-ABL fusion gene-positive precursor B-cell ALL.
The patient was put on treatment, i.e., chemotherapy – Levoflox 750 mg OD for 5 days, Septran DS alternate day BD (Wednesday and Saturday), Wysolone 100 mg OD, Imatinib 400 mg OD, tab. Forcan 400 mg OD, Pantop DSR OD, Chlorhex mouthwash, sitz bath TDS, betadine ointment, and tablet Zyloric 100 mg TDS.
The patient had also received 8 units of platelet-rich plasma and 8 units of packed red blood cells to improve the platelet counts and hemoglobin levels, respectively. The patient is responding well and now is off the alcohol. On follow-up visits, hematological parameters are also improving.
DISCUSSION
Available data on ALL in older patients are relatively sparse. One population-based registry reported that 31% of all cases occurred in patients 60 years or older although ALL is most common malignant disease in childhood while it is rare in adults.[8] Here, we had presented a case of 50-year-old male.
Most of patients with B-ALL present with evidence and consequences of bone marrow failure; thrombocytopenia, anemia, and neutropenia. The leukocyte count may be decreased, normal, or markedly elevated. Lymphadenopathy, hepatomegaly, and splenomegaly are frequent. Bone pain and arthralgia may be prominent symptoms.[9] Unusual presentation about our case was that he attended psychiatry OPD with motive of deaddiction of alcohol; chief complaints were generalized weakness and pain in legs which might be due to chronic dependence of alcohol. There was no evidence of any organ involvement such as hepatomegaly and lymphadenopathy. Neither the patient complained of any bone pain nor arthralgia. On complete blood count examination, counts were within normal limits initially.
B-ALL with BCR-ABL1 is relatively more common in adults than in children, accounting for about 25% of adult ALL but only 2–4% of childhood cases.[9] In our case also, the patient was middle-aged male.
CONCLUSION
We report this case with the intention of promoting greater awareness that ALL can cause significant unusual presentations without other systemic symptoms. Patients should be thoroughly examined and investigated for proper diagnosis; treatment can be started as early as possible to prevent fatal life-threatening complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Epidemiology of childhood cancer in India. Indian J Cancer. 2009;46:264-73.
- [CrossRef] [PubMed] [Google Scholar]
- Current concepts in pediatric Philadelphia chromosome-positive acute lymphoblastic leukemia. Front Oncol. 2014;4:54.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia in adults: A broader range of options, improved outcomes, and more therapeutic dilemmas. Am Soc Clin Oncol Educ Book. 2015;35:e352-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical outcome of children with newly diagnosed Philadelphia chromosome-positive acute lymphoblastic leukemia treated between 1995 and 2005. J Clin Oncol. 2010;28:4755-61.
- [CrossRef] [PubMed] [Google Scholar]
- Improved early event-free survival with imatinib in Philadelphia chromosome-positive acute lymphoblastic leukemia: A children's oncology group study. J Clin Oncol. 2009;27:5175-81.
- [CrossRef] [PubMed] [Google Scholar]
- Imatinib after induction for treatment of children and adolescents with Philadelphia-chromosome-positive acute lymphoblastic leukaemia (EsPhALL): A randomised, open-label, intergroup study. Lancet Oncol. 2012;13:936-45.
- [CrossRef] [Google Scholar]
- Long-term follow-up of imatinib in pediatric Philadelphia chromosome-positive acute lymphoblastic leukemia: Children's oncology group study AALL0031. Leukemia. 2014;28:1467-71.
- [CrossRef] [Google Scholar]
- National Cancer Institute, Surveillance, Epidemiology, and End Results Program. Available from: http://www.seer.cancer.gov [Last accessed on 2015 Jan 09]
- [Google Scholar]
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, eds. WHO Classification of Tumors of Hematopoietic and Lymphoid Tissue (4th ed). France: International Agency for Research on Cancer; 2017.







