Translate this page into:
Experiences with development and use of simulation-based module for teaching family study skills to undergraduate medical students in coronavirus disease epoch

*Corresponding author: Tanvir Kaur Sidhu Department of Community Medicine, Adesh Institute of Medical Sciences and Research, Bathinda, Punjab, India. sidhutanvir@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sidhu TK, Kaur P, Mehra S, Prajapati PR, Sidhu GS, Singh N, et al. Experiences with development and use of simulation-based module for teaching family study skills to undergraduate medical students in coronavirus disease epoch. Adesh Univ J Med Sci Res 2021;3(1):25-33.
Abstract
Objectives:
The objectives of the study were (1) to develop and validate a structured module for teaching family study skills through simulation to undergraduate medical students, (2) to train the undergraduate medical students using the module, (3) to obtain student’s perception regarding the module, (4) to obtain faculty perception regarding the module, and (5) to assess the students’ gain in knowledge and skills.
Materials and Methods:
The study was conducted as a participatory action research design with mixed-method approach in the Department of Community Medicine. A structured module was developed by the core committee and then internally validated. The teaching of family study skills was done using the structured module through online mode to 150 UG students (MBBS) of Phase 3. The perceptions and feedback of the students and faculty were collected and analyzed. The students were assessed for the gain in knowledge and skills. The thematic analysis was done for the feedback of students and faculty. Necessary changes and suggestions were incorporated at the end and the module is planned to be sent for external validation to subject experts. Both quantitative and qualitative analysis was done. For Likert scale data, median and IQR were used. Percentages were calculated for satisfaction reporting. Thematic analysis was done for open-ended questions.
Results:
The structured and internally validated module was created for training of UG students in Family study skills. The module was successfully pilot-tested for delivery through the online mode. The satisfaction of students was found to be >75% on all domains of the Likert questionnaire used for obtaining feedback. The faculty satisfaction was found to be >90%. Majority of the students scored satisfactory grades (88%) in the summative evaluation done at the end of the module. Both the faculty and students reported good experience with the new innovative TL methodology adopted, however, emphasized the non-replacement of real field learning experience. Nonetheless, it was acknowledged as the best solution in the era of social distancing.
Conclusion:
A structured validated module using simulation-based teaching-learning methods was successfully pilot tested to impart family study skills to undergraduate students through online mode. The simulation-based technology can be used for online teaching in the subject of community medicine during difficult times to supplement the physical teaching sessions.
Keywords
Community medicine
Coronavirus disease epoch
Family study skills
Simulation-based teaching
Structured module
INTRODUCTION
The competency-based medical education (CBME) curriculum has envisaged the acquiring of certain competencies through the community medicine curriculum, which contributes to instilling in knowledge, skills, and attitude in a budding doctor.[1] From the beginning, the separate study block for community medicine has been used for creating balance between clinical medicine, basic science, and community medicine in curriculum. Clinical social medicine, as seen in primary health care, cannot be taught in another setting as it does not exist elsewhere.[2]
The teaching-learning methodologies of these competencies are mostly based in the field practice area. Field experience and community learning are indispensable for building a foundation into a competent IMG. The teaching of these skills has been done through the Family study methodology adopted by almost all the colleges throughout the country since long. Teaching family-centered health care is an important facet of medical education. Families are being used as faculty to teach first-person family-centered care.[3] Community-based teaching through family visits is the core of medical graduates’ training.[4]
The 4 weeks of clinical posting in 3rd, 4th, and 6th Semester have been used for field training through allotment of families. The departments have been using clinico-psycho-social case studies or family presentations to focus on this clinical training. These are typical clinical case presentations with an added description of family members, socioeconomic status, dietary history, and household environment.
Adapting the framework of the Commission of Social Determinants of Health, a family study should: [5]
Identify the composite determinants of health affecting the particular family
Show how the major determinants relate to each other
Clarify the mechanisms by which these determinants act to decrease health
Provide a framework for evaluating which of these are the most important to address and map specific interventions for improvement of the health of the family.
Just like an index case (patient) is an entry point into a family, a family is an entry point into the community. Therefore, we also use the family study to gain insight into the larger health issues in the community. The appreciation of the economic, social, environmental, and emotional aspects in the medical problems should result in a change in their attitude and approach to patients. The end-point of a family study is a presentation made to faculty members. Usually, the focus of presentation and questioning is on the method of data collection, especially on clinical methods and dietary history. Evaluation of a family study includes equal weightage to the aspects of data collection, making diagnoses, web of interaction, and management.[6]
For more than a decade, medical schools have been working to transform pedagogy by eliminating/reducing lectures; using technology to replace/enhance anatomy and laboratories; implementing team-facilitated, active, and self-directed learning; and promoting individualized and interprofessional education.[7]
With the coronavirus disease 2019 (COVID-19) pandemic and its resultant concerns of social distancing, teaching family study skills became a big problem for the Department of Community Medicine. Even today, when we are at a decrease in the absolute numbers, the free interaction of students into community remains a challenge. Due to this alternative way of delivering these learning experiences became the need of the hour. The use of simulation was one answer.
Although simulation in medicine has been in vogue since the 9th century when Madame du Coudray used mannequin pelvis and babies to train midwives for childbirth, its use became more rampant with the introduction of versatile human simulators by the late 1990s and early 2000s. Simulation has been used in training for the Departments of Anesthesia, Pharmacology, Physiology, Surgery, and Pediatrics to name a few for quite some time,[8,9] but their use in Community Medicine to replace actual field experience has never been tried. Few studies on using simulation in public health have developed pre-analysis framework for network-based epidemic simulations for purposes of training students and novice researchers and gave framework reduction and extension examples in terms of collected geographic and demographic data.[10]
Simulation is an educational strategy in which a particular set of conditions is created or replicated to resemble authentic situations that are possible in real life. Simulation can incorporate one or more modalities to promote, improve, or validate a participant’s performance.[11] Simulation if properly planned has been studied to address the educational needs and domains as represented in the following Figure 1.[11]
- Domains addressed by Simulation models
Simulation-based experience(s) are a broad array of structured activities that represent actual or potential situations in education, practice, and research. These activities allow participants to develop or enhance knowledge, skills, and/or attitudes and provide an opportunity to analyze and respond to realistic situations in a simulated environment.[11] One way of simulation is use of standardized patient (also known as simulated patient). He is a person trained to consistently portray a patient or other individual in a scripted scenario for the purposes of instruction, practice, or evaluation.[11]
Some guidelines are crucial while developing any simulation-based learning sessions. These include: – Performing a need assessment, developing learning objectives, structure the format, designing a case scenario of the context, create realism, facilitate the participant, pre-briefing, debriefing, evaluation of all involved and feedback session, provide resource and preparation material, and finally pilot test.[12]
While online teaching has taken up most of the current learning platform, the teaching of these family skills cannot be compromised and has to continue even in the current scenario. There might arise a need to continue similar methodologies of training in the few years to follow. With this background in mind, the present study was planned for training undergraduate students of our medical institution to expose the students to community learning.
Hypothesis
Use of a structured training module using simulation techniques can aid teaching family study skills to undergraduates in times of social distancing.
Aim
The aim of the study was to teach family study skills through simulation-based methods.
Objectives
The objectives of the study were as follows:
To develop and validate a structured module for teaching family study skills through simulation to undergraduate medical students
To train the undergraduate medical students using the module
To obtain student’s perception regarding the module
To obtain faculty perception regarding the module
To assess the students’ gain in knowledge and skills.
MATERIALS AND METHODS
Study design
This study was participatory action research using mixed research methods.
Setting
Adesh Institute of Medical Sciences and Research, Bathinda, Punjab
Department of Community Medicine
Clinical Posting- Online mode.
Participants
Undergraduate MBBS students (Phase 3).
Sampling
Complete enumeration (all 150 students in batches of 30, posted in clinical posting).
After obtaining Research approval and Ethics approval, a Departmental Core-Committee (CC) of seven faculties was constituted, sensitized, and individual consent was sought. The CC then identified the various sub-topics and related skills to be taught through family study according to the specified curriculum guidelines of university.
The CC finalized a template for preparing lesson plan for each session. Each member was made in charge of one sub-topic and allotted the responsibility to design and prepare resource material for the session. Each session was then discussed in the CC, 1 week before delivery and feedback/ suggestions were incorporated to internally validate. This was followed by internal validation of the module by the Core Committee members and compilation was done by the main researcher.
After Internal validation, the lesson plan was distributed to all faculty who conducted the SBT session for 30 students each. The MBBS students rotating in online clinical classes for Community Medicine were trained using the module from October 17 to December 12, 2020 (2 h daily for 8 days–16 h). The Online teaching platform of the institution was used for conducting online workshops and permission was obtained for the same. A Google classroom was created to share the resource material. Informed written consent was obtained according to the requirement of the Ethics Committee as a part of the pro forma before recruiting the students.
The data collection tools consisting of feedback questionnaires and assessment forms were prepared using the extensive literature search and validated by the CC internally. Data collection was done through Google forms shared through Google classroom. A total of 144 students who attended the entire training were considered for data analysis. A total of 7 resource faculties who were part of the CC were involved in delivering the workshop. The formative assessment of the students was also conducted at the end of each session. The summative assessment was conducted at the end of the complete module.
Necessary changes and suggestions were incorporated at the end and the final module is planned to be sent to experts for external validation (Subject experts and medical education experts outside the institution).
Data collection from students
Feedback was collected from the students on the last day of the posting after explaining about the study and getting written informed consent using both quantitative and qualitative method.
The summative assessment was conducted at the end of the posting of the whole batch.
Data collection from faculty
Feedback from the resource faculty and core committee by collected using questionnaires at the completion of the training after getting written informed consent.
Data were entered in Microsoft excel 2010 and quantitative data were analyzed. Descriptive statistics included percentages and median. Themes were identified for the responses to open-ended questions and content analysis done for the faculty feedback.
RESULTS
The validation of the module was established by the internal experts on face and content validity parameters. The face validity was established based on the format and presentation of the module. The face validity was reported to be satisfactory (>70% on all items). The content validity was measured on various sub-criteria using individual items. The overall module content validation index (CVI) was found to be 0.95 and universal agreement (CVI-UA) was 0.75.
Outline of the developed module
The module was prepared to be delivered in 7 sessions, namely Community Diagnosis (2 h), family biodata and socio-economic status (2 h), environmental assessment (2 h), nutritional assessment (3 h), immunization (2 h), KAP study including family planning (2 h), and clinico-social cases (3 h). The learning objectives of each session were planned with the TL methods; resources and assessment to be used were outlined.
The various LOs session-wise are detailed as below. At the end of the session, the student should be able to:
Community diagnosis
Define “Community”
Define “Community Diagnosis” and enumerate steps in community diagnosis
Generate Community Diagnosis for the given Case Scenario.
Family biodata and socio-economic status
Define “Family and its types”
Identify “Head of the family”
Discuss the importance of family biodata (address, religion, caste)
Discuss and apply the various types of socio-economic scales
Generate family biodata profile along with the socioeconomic status for the given family scenario.
Environmental assessment
Draw a MAP of house of allotted family
Assess and analyze the outdoor and indoor environment of allotted family
Asses sanitary and housing conditions
Identify overcrowding if present or not in allotted family
Assess the adequacy of ventilation in that house
Assess the biological and psycho-social environment of the house
Comment on water supply and distribution of water in the house
Identify and comment on environment related models
Bring positive change in knowledge, attitude, and practices related to environment in allotted family.
Nutritional assessment
Describe the role of nutrition in human health
Classify various food items on the basis of their nutritional values
Identify the nutritional needs of the family
Calculate the nutritional intake of the family
Estimate the nutrition gap
Formulate a diet plan to fill the gap
Counsel the family/provide nutritional education.
Immunization
Describe the national immunization schedule under UIP (Universal Immunization Program)
Enlist the new vaccines introduced under UIP (Universal Immunization Program)
Recommend the immunization schedule according to the various case scenarios for vaccination of a child/ pregnant women
Identify and demonstrate the usage of various equipment’s used under “Cold Chain.”
KAP study including family planning
Discuss and distinguish knowledge, attitude, and practices
Illustrate KAP of NCD and CD
Illustrate KAP of immunization, child birth, breast feeding and family planning
Identify the KAP gap
Demonstrate different ways (counsel, education) to fill this KAP gap.
Clinic-social cases
Illicit history related to possible cases in the family
Formulate clinical diagnosis after history and physical examination
Formulate social diagnosis considering physical, biological, and social environment of the case and the family
Design and deliver a comprehensive management plan
Deliver health education and counseling related to the case.
Activities planned to meet these objectives
Community diagnosis, community walk, knowing your link workers, data collection and recording, generating community diagnosis, family, head of the family and types of family, family biodata details, types of socio-economic scales and role of socio-economic status in health and disease, data collection and recording, generating family bio data and assessing their socio-economic status, introduction to physical environment and related health, assessment of housing; including ventilation and overcrowding of the house, assessment of water supply and distribution, assessment of sanitary conditions, assessment of biological and psycho-social environment, report preparation and presentation, describe the role of nutrition in human health, classify various food items on the basis of their nutritional values, identify the nutritional needs of the family, calculate the nutritional intake of the family, estimate the nutrition gap, formulate a diet, plan to fill the gap, provide nutritional counseling, introduction and history of immunization, national immunization schedule with vaccine dose and site, route of administration, etc., equipment of cold-chain, eliciting immunization history from the mother of an under 5 children, various case scenarios of partially/un-vaccinated child/pregnant women, introduction of KAP concept and its importance, identify KAP in NCD and CD, identify KAP in Immunization, child birth, breast feeding, identify KAP in family planning, prepare questionnaire to know KAP gap and suggestive ways to fill the gap, Elicit KAP history from simulated patient, demonstration of counseling/Health education on the identified gap area, identification of cases in the family-history taking, physical examination, generate comprehensive diagnosis, design management plan, demonstrate counseling/health education and finally debriefing, and feedback and reflections.
Various TL methods and resources used
Observation and report preparation of the video, followed by presentation by the students, recording the data and submission, case- based learning, PPT, simulated video on community walk, recorded video interviews with the health workers, Pro forma – Community Profile (Family Record Book), paper based case scenario, interactive session, briefing regarding various types of socio-economic scales and their uses, observation and report preparation from the videos, checklist pro forma, self-exercise to calculate socio-economic status of one’s own biological family, recorded video interview with family + Pro forma – family bio data and socio-economic status of the family (family record book), simulated patient interview by students using breakout rooms, interactive lecture, brainstorming, DOAP (role play), building a sketch map, SGD, AV aids, Video links, simulation exercise, simulated role play, simulated family, One’s own biological family, maids families, simulated mother of an under 5 child, case scenarios discussion, Chalk and Board, Zoom breakout rooms, printed case exercises, allotment of topic to groups, and simulated patient and case taking.
The various assessment methods used were: evaluation and feedback for the submitted case sheet, assessment of the environmental reports prepared by students, case presentation-nutritional assessment and diagnosis, including counseling and nutritional education, case based scenario, and simulated case presentations.
The sessions were held consequently using the module through the online mode and feedback of the students was obtained on Likert scale (ranging from 1 to 5). This is depicted as in [Table 1].
| Topics | Median | IQR |
|---|---|---|
| Community diagnosis | 4 | 3–4 |
| Family biodata and socio-economic status | 4 | 4–5 |
| Environmental assessment | 4 | 3–5 |
| Nutritional assessment | 4 | 4–5 |
| KAP and family planning study | 4 | 3–5 |
| Immunization | 4 | 4–5 |
| Clinicosocial case discussion | 4 | 3–5 |
| Overall satisfaction | 4 | 3–4 |
IQR: Interquartile range
[Table 1] shows that the median of satisfaction level of participants for all attended family study sessions is 4 (highly satisfactory) and interquartile range for most of the sessions lies between 3 and 5.
The satisfaction percentages of students with various sessions as well as overall satisfaction are shown as in [Figures 2 and 3].
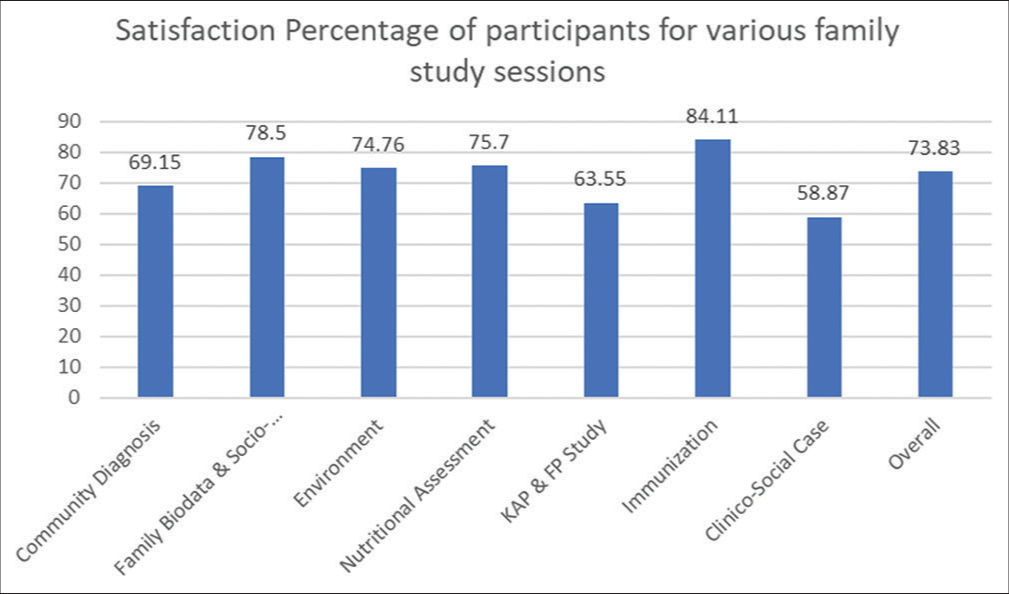
- Satisfaction percentage of students.

- Overall satisfaction of students.
Thus, the overall satisfaction level was high in majority of students.
[Table 2] shows that the median of rating of students on various variables of the sessions is 4 (highly satisfactory) and interquartile range for most of them lies between 3 and 4.
| Variables | Median | Inter Quartile Range |
|---|---|---|
| Learning objectives | 4 | 3-4 |
| Scientific content and resource material | 4 | 3-4 |
| Teaching leaning methodology and assessment used | 4 | 3-4 |
| Guidance/facilitation provided by faculty | 4 | 4-5 |
| Overall learning experience | 4 | 3-5 |
Figure 4 shows that overall learning experience of the participants for the whole block of the family study was good.
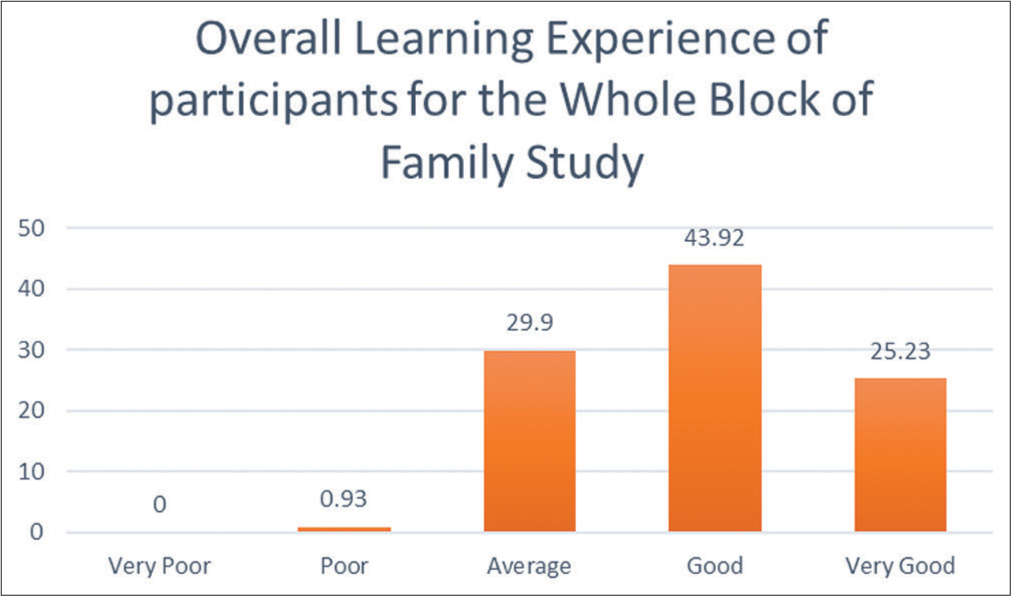
- Overall learning experience of students.
Similarly, feedback was obtained from faculty on Likert scale on the variables to rate the teaching block.
[Table 3] shows that the median of rating level by the faculty members for family study sessions is 4 and interquartile range lies between 4 and 4. About 100% faculty was satisfied with the overall teaching experience.
| Variables | Median | Inter quartile range |
|---|---|---|
| Learning objectives | 5 | 5–5 |
| Scientific content and resource material | 4 | 4–5 |
| Teaching leaning methodology and assessment used | 4 | 4–4 |
| Student participation | 3 | 2–4 |
| Overall teaching experience | 4 | 4–4 |
Thematic analysis was done for the open-ended questions. Themes generated on qualitative analysis of the student and faculty feedback is depicted as in [Figures 5 and 6] for students and faculty, respectively.

- Themes generated after qualitative analysis of feedback provided by students.

- Themes generated after qualitative analysis of feedback provided by faculty.
The students were assessed on a global rating scale after the training. About 87.5% students were able to satisfactorily perform in the assessment conducted by the faculty after 2 weeks. The performance is shown in [Figure 7].
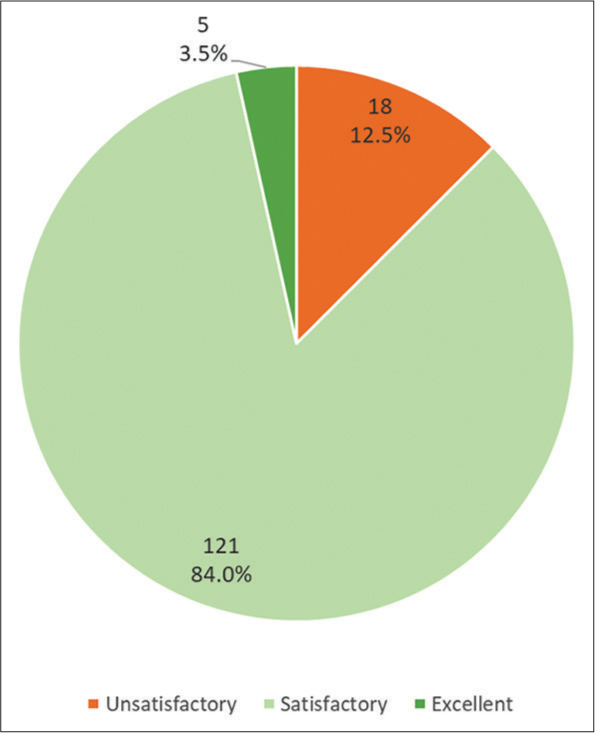
- Pie diagram showing performance of students.
Out of total 144 students, 18 (12.5%) scored unsatisfactory, 121 (84%) scored satisfactory, and 5 (3.5%) students excelled with excellent scoring.
DISCUSSION
A structuring approach to teach family study skills has been tried by authors in the past. Around 11 domains were identified by a study conducted by Krishnan et al. in 2017.[6] In our study, we identified 7 domains under which the sessions were delivered and the final assessment approach was similar as in the referred study. The seven subtopics were structured with substituting the field visits by the various teaching-learning methodologies. The students were asked to work on their own personal families as a simulated family and generate all the relevant data related to them. The students worked on family demographic structure, socio-economic status, environmental assessment, nutritional assessment of family, and then all members, conducting KAP sessions on their family members with detailed communication recordings and immunization workouts. This was followed by the generation of clinic-social diagnosis and then generating an action plan. The teaching training methods used for simulation exercises were simulated patients/standardized patients, role plays, virtual tours, pre-recorded interviews with families/patients/ health workers, etc., and case-based learning exercises.
In the scenario of complete absence of field visits to families in the COVID situation, the student teaching training program was continued with the creation of the best possible alternatives to simulate the community setting experiences. Although the actual experience cannot be replaced, the students were largely satisfied with the efforts made by the faculty to teach family study. About 74% students were satisfied with more satisfaction being accorded to the teaching of immunization sessions, followed by biodata, socio-economic status, environmental, and nutritional sessions. The lowest satisfaction was reported for clinic-social cases as expected since we know that the actual case-taking experience is difficult to be replicated in controlled settings.
The overall satisfaction with the learning experience was about 70 % and around 30 % was average. Only 0.93% were not satisfied. The students reported satisfaction to clearly defined learning objectives, resource material provided, TL methods used, and assessment and were completely satisfied with the guidance provided by the faculty.
The teachers were 100% satisfied and had put maximum effort to achieve high-quality learning environment for students. However, they reported student participation to below.
The thematic analysis of the students and faculty responses to open questions was done. The positive aspects of the initiative were brought about nicely by the students and faculty. The problem areas were also identified, however at the same time, suggestions were made to overcome them. Some of the verbatims of the faculty are:
“the skills taught this way can help them for their actual interaction with community…”
“develop more videos for showing interaction with community…”
“…. help in communication skill development…”
“formative assessment and feedback improve students’ active participation and learning…”
The final crux that emerged was that simulated family study teaching was the only option of preventing the academic loss to the students in the COVID epoch. The use of technology and structuring of lessons by the faculty was the landmark innovation which worked successfully and was feasible and acceptable to both the teacher and the learner.
The profound effects of COVID-19 may forever change how future physicians are educated.[7] The module is here to stay in case of any such future needs and can also be taken up for priming the students before taking up actual field sessions in the future. More and more resource generation can be done by collaborating with other departments/colleges and universities for validating this further.
CONCLUSION
A structured validated module using simulation-based teaching-learning methods was developed to impart family study skills to undergraduate students through online mode. The module was pilot tested and students and faculty were satisfied with the teaching using the developed module
The simulation-based technology can be used for online teaching in the subject of Community Medicine during difficult times to supplement the physical teaching sessions.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Competency Based Undergraduate Curriculum for the Indian Medical Graduate. 2018. India: Medical Council of India; Vol 2:41-59. Available from: https://www.nmc.org.in/wp-content/uploads/2020/01/ug-curriculum-vol-ii.pdf [Last accessed on 2021 Mar 23]
- [Google Scholar]
- Eight years experience from the University of Tromso. Scand J Prim Health Care. 1986;4:109-14.
- [CrossRef] [PubMed] [Google Scholar]
- Using families as faculty in teaching medical students family-centered care: What are students learning? Teach Learn Med. 2006;18:222-5.
- [CrossRef] [PubMed] [Google Scholar]
- Family health study: Core of public health practice. 2005. Indian J Community Med. 30:99. Available from: https://www.ijcm.org.in/text.asp?2005/30/3/99/42863 [Last accessed on 2021 Jan 25]
- [CrossRef] [Google Scholar]
- A Conceptual Framework for Action on the Social Determinants of Health: Discussion Paper for the Commission on Social Determinants of Health Geneva: Commission on Social Determinants of Health; 2007.
- [Google Scholar]
- Approach to family assessment and intervention. 2017. Natl Med J India. 30:279-84. Available from: http://www.nmji.in [Last accessed on 2021 Jan 23]
- [CrossRef] [PubMed] [Google Scholar]
- Medical student education in the time of COVID-19. JAMA. 2020;323:2131-2.
- [CrossRef] [PubMed] [Google Scholar]
- Simulation in healthcare education: A best evidence practical guide. AMEE Guide No. 82. Med Teach. 2013;35:e1511-30.
- [CrossRef] [PubMed] [Google Scholar]
- Simulations for epidemiology and public health education. J Simul. 2010;4:68-80.
- [CrossRef] [PubMed] [Google Scholar]
- INACSL standards of best practice: Simulation SM Simulation glossary. Clin Simul Nurs. 2016;12:S39-47.
- [CrossRef] [Google Scholar]
- Pros and cons of simulation in medical education: A review. Int J Med Health Res. 2017;3:84-7.
- [Google Scholar]







