Translate this page into:
Thoracic spine extradural hematoma secondary to thrombotic thrombocytopenic purpura: A case report

*Corresponding author: Otávio da Cunha Ferreira Neto, Center of Biological Sciences and Health, Catholic University of Pernambuco, Recife, Pernambuco, Brazil. otaviocferreiraneto@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ferreira Neto O, Diniz AM, Alencar Neto JF, Lemos NB, Marques LF, Neto LB, et al. Thoracic spine extradural hematoma secondary to thrombotic thrombocytopenic purpura: A case report. Adesh Univ J Med Sci Res 2022;4:109-11.
Abstract
Thrombotic thrombocytopenic purpura is a rare but a fatal disease with a life-threatening thrombotic microangiopathy. We report a case of 35-year-old male, admitted with abdominal pain and fever, growing into progressive crural spastic paraparesis level II, and urinary retention. On investigations, thoracic MRI showed an extradural hematoma in thoracic spine between T11 and L1 and spinal compression. After 5 days of treatment with glucocorticoids, clinical picture got better. In this condition, we decided to have non-surgical intervention. The literature says that the true correlation between severe thrombocytopenia and spine epidural hematoma formation is unknown due to limited data.
Keywords
Extradural hematoma
Thrombocytopenic purpura
Hematology
Thoracic spine hematoma
Neurosurgery
INTRODUCTION
Thrombotic thrombocytopenic purpura (TTP) is a rare but highly fatal thrombotic microangiopathy entity, defined by a severe deficiency in ADAMTS13 (a Disintegrant and Metalloprotease with eight Thrombospondin-1-like), which degrades von Willebrand factor (VWF). Low concentrations of ADAMTS13 facilitate thrombus formation, resulting in organs’ ischemia and failure.[1,2] Kidneys and central nervous system (CNS) are the most affected systems by TTP which is characterized by widespread thrombosis.[1,2]
Signs and symptoms of TTP reflect thrombocytopenia and hemolytic anemia underlying end-organ injury. Hemolytic anemia can present with fatigue or dyspnea and thrombocytopenia may present as mucosal bleeding, petechial, and/or purpuric skin rash. Manifestations in the CNS can include headache, focal neurologic deficits due to bleeding or ischemia, seizures, confusion, fever, and vertigo.
The “classical” clinical pentad for diagnosing TTP includes – thrombocytopenia, platelet count <150 000/μL; microangiopathic hemolytic anemia (MAHA), defined as a hemoglobin level <13.5 g/dL in men or <12 g/dL in women, with two or more schistocytes per field in the peripheral smear; increased serum lactate dehydrogenase (LDH) above upper normal laboratory range; normal clotting tests; and negative direct Coombs’ test.[3] TTP constitutes a medical emergency with high mortality, if the early diagnosis is not done.[3,4]
At present, limited data exist about the risk of spinal epidural hematoma (SEH) in severely thrombocytopenic patients. SEH can be a complication of thrombocytopenia and can result in permanent neurologic deficits.
CASE REPORT
Male patient, 35 year old, was admitted with history of abdominal pain, diarrhea, and 5 days of fever. On the 3rd day of admission, the patient presented with mental confusion, grade 2 spastic paraparesis and urinary retention. Laboratory results showed platelet count of 20,000/μL, 9 g/dL hemoglobin, 2.000 U/L LDH, and 7 mg/dL bilirubin. He also presented with non-specific viral symptomatology 7 days after his admission and was tested for COVID-19 and HIV, both negative. In the face of thrombocytopenia, MAHA, serum LDH levels, neurological focal signs and symptoms, and fever, the patient was diagnosed with TTP and was treated with plasmapheresis for 7 days.
A thoracic MRI showed an epidural hematoma dorsally on thoracic spine beginning on T11 and extending to L1, causing medullary compression [Figures 1 and 2]. Immediate surgical evacuation of hematoma was not considered as first option since PTT has good response to corticosteroids. After 5 days of methylprednisolone, the patient was clinically better, and a new control thoracic MRI showed hematoma reabsorption.
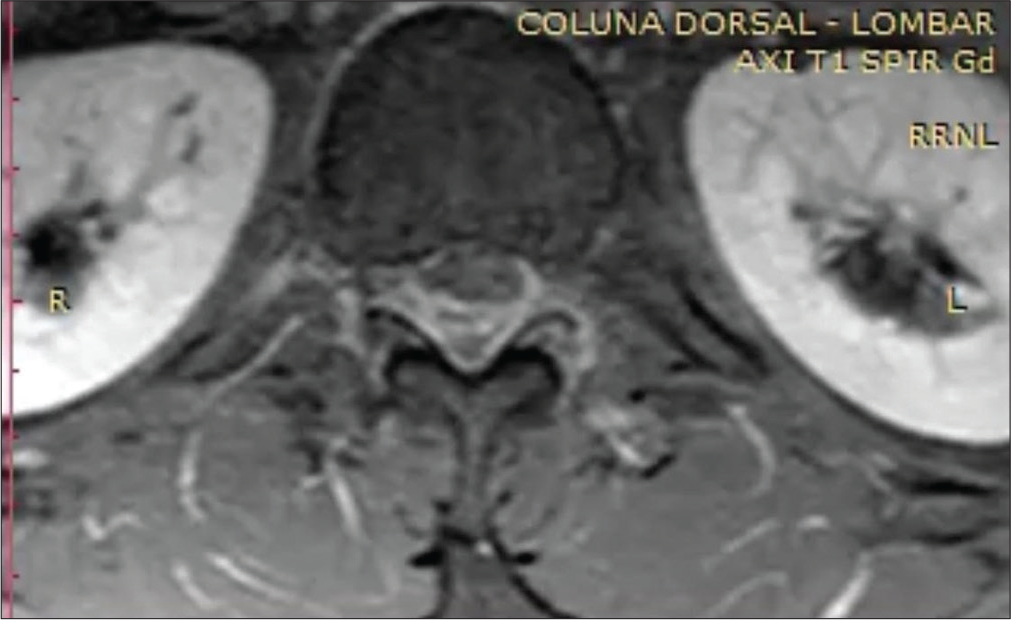
- A 35-year-old man male with an extradural hematoma in thoracic spine with abdominal pain and fever. Axial image of an MRI of the thoracic spine, T1-weighted.

- A 35-year-old man male with an extradural hematoma in thoracic spine with abdominal pain and fever. Sagittal MRI of the thoracic spine, T1-weighted.
DISCUSSION
TTP pathophysiology consists in a deficiency in ADAMTS13, a protein that cleaves vWF multimers released by endothelial cells. When the enzymatic activity of ADAMTS13 is severely reduced usually below 10%, vWF multimers accumulate on the endothelial surface, favoring platelet aggregation and thrombotic microangiopathy. In adults, almost 90% of TTP cases are acquired and mostly idiopathic, with patients having circulating immunoglobulin G antibodies against ADAMTS13. Factors associated with secondary TTP include pregnancy, autoimmune disorders, certain drugs, neoplasms, transplantation, and infections, like human immunodeficiency virus (HIV).[3]
To this day, there are scarce papers and articles on PPT and CNS hemorrhages. In our search, the first article discussing the matter was a case report about a patient that was admitted with a 3-day temporal headache associated with nausea. Initial thoracic MRI showed a frontotemporal subdural hematoma and laboratory results were consistent with idiopathic thrombocytopenic purpura. The patient also presented with gingival hemorrhage, melena, epistaxis, and menorrhagia. He was later transferred to the hematology unit to evaluate treatment options due to persistent low platelet counts. Splenectomy was later performed which increased platelet number and made possible the interruption of corticosteroids.[5]
CONCLUSION
This case report illustrates one of the few examples when surgical evacuation of an epidural spinal hematoma visualized on thoracic MRI is not the best treatment option. A patient presenting with laboratory results consistent with TTP, even with a SEH and established motor deficit for more than 48 h may benefit from clinical treatment as proved in our experience. There are still limited data to prove the true correlation between severe thrombocytopenia and SHE development.
Acknowledgments
We are grateful to the masters who provided insight and expertise that greatly assisted the research and actively stimulated the search for answers.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Thrombotic thrombocytopenic purpura: Beyond empiricism and plasma exchange. Am J Med. 2019;132:1032-7.
- [CrossRef] [PubMed] [Google Scholar]
- An update on pathogenesis and diagnosis of thrombotic thrombocytopenic purpura. Expert Rev Hematol. 2019;12:383-95.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical presentation in thrombotic thrombocytopenic purpura: Real-world data from two Mexican institutions. J Clin Apher. 2018;33:645-53.
- [CrossRef] [PubMed] [Google Scholar]
- Thrombotic thrombocytopenic purpura In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2021.
- [Google Scholar]
- Hematoma subdural bilateral frontotemporal em PTI: relato de caso. Rev Med. 2017;96:204-8.
- [CrossRef] [Google Scholar]








