Translate this page into:
Physiotherapy in upper-limb tourniquet palsy

*Corresponding author: Mubarak Muhammad Yahaya, Department of Physiotherapy, Abubakar Tafawa Balewa University Teaching Hospital, Bauchi, Nigeria. mubarakyahya30@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yahaya MM, Jawa BK, Saleh BC. Physiotherapy in upper-limb tourniquet palsy. Adesh Univ J Med Sci Res. 2024;6:106-11. doi: 10.25259/AUJMSR_1_2024
Abstract
Upper-limb tourniquet palsy is an unusual complication of upper-limb surgery that needs immediate physiotherapy intervention. It occurs, when tourniquet is applied for high pressure or extended duration more than recommended, leading to nerve injuries and other complications which need immediate attention to prevent disabilities. This is a case of 35-year-old patient diagnosed with tourniquet palsy following right midshaft radius and ulnar fracture and reduced by open reduction and internal fixation where the surgery lasted for <1½ h but diagnosed a few days later with radial, median, and ulnar nerve injury. Following aggressive physiotherapy intervention daily for 8 weeks, the patient remarkably recovered. Aggressive and early physiotherapy treatment was found to improve pain, muscle power, functional abilities, and activities of daily living in patients with upper-limb tourniquet palsy.
Keywords
Nerve injury
Palsy
Therapeutic ultrasound
Tourniquet
INTRODUCTION
A pneumatic tourniquet is a device that is widely used to control blood flow to distal part of the upper or lower limb during a surgical procedure to limit bleeding and give a clear surgical field.[1] The evolution of tourniquet starts from simple cloth bands tied tightly around limbs to mechanical screw tourniquets, to elastic, non-pneumatic Esmarch tourniquets and then to pneumatic ones that were developed by Harvey Cushing in 1904 and most recently, to the current generation of microprocessor-controlled pneumatic tourniquets first conceived and developed by Masri et al.[1,2]
However, application of a tourniquet for long hours or too tight results in undesired outcomes ranging from paresthesia to paralysis due to injury to the nerves by direct compression against the bone and radial nerve is mostly affected, followed by ulnar and median nerve,[3] muscles injury as a result of ischemic changes, skin and vascular injuries.[1,3]
With the introduction of pneumatic tourniquet technology, the frequency and severity of complications reduced than in non-pneumatic elastic tourniquets, which produced uncontrolled pressure resulting in nerve injuries and pulmonary embolism.[1,4]
Evidence reported that about 60.2% of orthopedic surgeon practice in Nigeria use non-pneumatic tourniquets and non-pneumatic ones are more fronts to cause nerve injuries to the patient, which can lead to paralysis.[5] It was also seen that 2 out of 5 post-operative complications related to tourniquet use for 108 min duration cause nerve injuries (neuropraxia), and patients present with palsy that usually resolve within 6 months.[6]
Tourniquet palsy is an uncommon complication of orthopedic surgical procedures and only a few researchers reported the incidence in Nigeria, and few among published articles reported the role of physiotherapy in facilitating the recovery of functional abilities in patients with such conditions. This case report will provide an insight about the benefit of systematic and aggressive physiotherapy intervention in the management of tourniquet palsy following open reduction and internal fixation (ORIF).
CASE REPORT
A 35-year-old male civil servant was referred to the Physiotherapy Department by an orthopedic surgeon on account of right upper-limb paralysis following a surgical procedure.
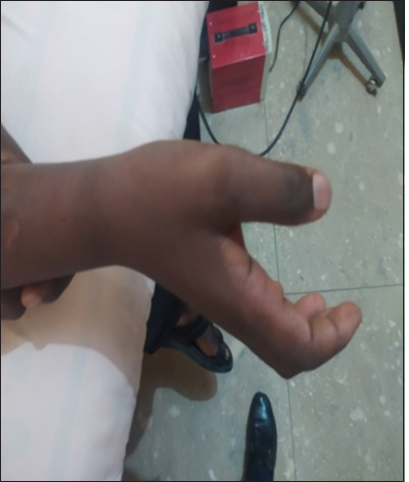
On the first assessment, the patient was on admission but before that, he was said to be in good health before he was involved in road traffic accident, he collided head-on with a tricycle while riding motorbike where he sustained fracture at right midshaft of ulna and radius [Figure 1] which was reduced by ORIF 2 days after admission [Figure 2]. A day after surgery, the surgeon reviewed and realized that patient could not flex and extend his elbow, wrist, and fingers of the right upper limb as a result of weakness.

- Fracture at right midshaft of ulnar and radial bone.

- Post-operative X-ray (plate and screw).
On the neurological assessment of the patient, ulnar, median, and radial nerves of the right upper limb were found to be affected (neuropraxia), with relative loss of deep and light sensation of the right upper limb below the elbow joint; passive range of motion of right elbow and wrist joint was full to range but painful (numeric pain rating scale [NPRS]: 7/10); muscle bulk was preserved, normoreflexia of triceps and biceps tendon. Muscle power was also assessed using Oxford Muscle Grading Scale (OMGS) of the right shoulder. Flexors, extensors, and adductors which were found to be: Shoulder abductors and adductors were 3/5, elbow flexors and extensors were 1/5; and wrist flexors, extensors, ulnar deviators, and radial deviators were 1/5. The level of pain in the right upper limb on NPRS was 7 out of 10 and the Barthel index for activities of daily living (ADL) was found to be 70 points out of 100 and minimally dependent with limitation in feeding, bathing, grooming, and dressing and QuickDASH score was 84.1/100.
Aggressive physiotherapy treatment was planned for the everyday session including Saturdays and Sundays, inform of transcutaneous electrical nerve stimulation (TENS) with burst mode to right elbow flexors and extensors, wrist and fingers flexors and extensors at rate of 4.0 Hz, width 120 μs for 15 min in 2 sets (making 30 min) for pain and muscle strength. Gradual passive range of motion exercise to the elbow, wrist and fingers joints for 10 repetitions each/set, 5 sets/sessions and 1 session everyday. then, active assisted range of motion exercises to the elbow joints in flexion and extension direction and then against the gravity [Figures 3, 4 and 5], active pronation achieved after 24th visit [Figure 6] and arm-sling application is advised especially while standing to avoid swelling of fingers. . After 24th consecutive sessions (4 weeks), the pain reduced to 3/10 NPRS, there was improved muscle power of the shoulder complex to 4/5, elbow flexors and extensors improved to 2/5, and wrist and finger flexors and extensors to 2/5 of OMGS.

- Elbow flexion against gravity after few sessions.
- Attempt wrist joint antigravity movement in flexion or extension.

- Wrist extension after 24th sessions.

- Active pronation after 24th sessions.
Physiotherapy treatment sessions continue in the form of neuromuscular electrical stimulation to the right wrist and finger flexors and extensors at the rate of 50 Hz and width 120, 50 s, and 10 s of ON and OFF, respectively, for 30 min. Resistant exercises of the right elbow flexors and extensors using 2LB dumbbell [Figure 7] for 10 repetions/set for 5 sets/session, the same dosage of exercises (10 repetions of 5 sets) were used for range of motion exercise for the wrist joints and gripping exercise [Figure 8] for 7 weeks treatment period on alternate days.

- Resistant exercises with dumb bell.

- Active gripping exercise.
On review, the pain reduced to 1/10 NPRS, QuickDASH score was 27.3/100, and Barthel index of 100 points. Patients could actively flex and extend right elbow and wrist joints with resistance. He could also pick handball from the table and actively supinate and pronate his right forearms [Figures 9 and 10]. All the muscle groups were 4/5 and finger flexors and extensors were 4/5 on OMGS.

- Patient trying to take handball.

- Patient with handball and squizzing.
On subsequent follow-up at 10 weeks, patients can drive his motorcycle, write with the affected hand, and perform ADL with mild limitation, then he was given a home program and advised to continue once a week follow-up.
DISCUSSION
In a survey conducted at Annual General Meeting/Scientific Conference of Nigerian Orthopedic Association among orthopedic surgeons in 2021, 60.2% of the respondents usually used non-pneumatic tourniquet which put the patient at risk of complications not only to the nerves and muscles but also caused deep venous thrombosis, pulmonary embolism, wound healing problems, arterial thrombosis, multiple cardiac and cerebral emboli, skin irritation, compartment syndrome, post-tourniquet syndrome, and myonephropathic metabolic syndrome after tourniquet release.[5,3]
When an Esmarch tourniquet or any non-pneumatic tourniquet is being used, it is associated with high risk of morbidity but with the invention of pneumatic tourniquet and the recent production of microprocessor-controlled pneumatic tourniquet has the potentials in minimizing complications associated with using tourniquet but still, there is a chance of experiencing nerve or muscle injury that can cause paralysis.[2] Contrary to a study which reported that injury that led to paralysis was caused by prolonged application of the tourniquet for more than 2 h,[1,4] but this case study showed that the paralysis might be likely caused by excessive direct pressure from tourniquet because the time taken for the surgery was <1½ h.
In a study conducted in 2016 where 121 patients who underwent upper limb surgeries using tourniquet at an average time of 30 min–105 min, about 5 patients among the cases reported with 5 post-operative complications and 2 have nerve injuries inform of neuropraxia which resolved within 6 months and other 3 reported with tourniquet pain.[4,6] This is in the same vein with our case in which the tourniquet time was <1½ h and patients present with paralysis and pain.
Moreover, another case study published in 2021 showed remarkable improvement in patient’s functional abilities and pain following daily physiotherapy treatment sessions for 8 weeks before booked on a weekly visit, this is in line with our findings, which showed significant improvement in pain and muscle power after 7 weeks of daily physiotherapy treatment sessions as the patients can drive his motorcycle, write with the affected hand, and perform instrumented ADL with mild difficulties.[2]
Tourniquet pressure for more than 300 mmHg is reported to be sufficiently enough to cause nerve and muscle injuries and also other complications associated with nerve injury, likewise time frame for tourniquet application is considered one of the domains that usually leads to complication associated with upper-limb tourniquet palsy, especially when duration exceeds 2 h before releasing the tourniquet.[3,7,8] As such, moderating and monitoring the extent of tourniquet application pressure, time it takes and breaking the time is essential in preventing complication associated with tourniquet, In this case, pre-operative nurses and surgeon assistants should have knowledge at hand for preventing risks associated with tourniquet palsy.[2,3,8]
There is evidence that paralysis due tourniquet application resolves spontaneously in 6 months’ time (25 weeks), patient who underwent upper limb may find it difficult to return to work without rehabilitation, as such, patient will be at risk of developing much complications such as joint stiffness, muscles wasting, and loss of dexterity skills which will cause extra complication financially. With physiotherapy intervention and close monitoring, early and remarkable outcomes can be achieved as in this case where patient improved handsomely in <10 weeks.
When physiotherapy treatment sessions start as soon as when patient is diagnosed with tourniquet palsy and competent physiotherapist design aggressive treatment plan usually gives remarkable recovery and assists in early return of functional abilities and back to workplace which might reduce economic burden. In addition, it prevents permanent activity limitation and dependency.
Recommendations
Microprocessor-controlled pneumatic tourniquet is advised to be used as applicable as possible, close monitoring while using any other tourniquet and immediate assessment of nerve injuries is recommended. Physiotherapy treatment options play vital in early recovery and prevention of disabilities.
CONCLUSION
Upper-limb tourniquet palsy is an unusual complication of upper-limb surgery that needs immediate physiotherapy intervention, aggressive and early physiotherapy treatment was found to improve pain, muscle power, functional abilities, and ADL in patients with upper-limb tourniquet palsy.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Tourniquet-induced nerve compression injuries are caused by high pressure levels and gradients-a review of the evidence to guide safe surgical, pre-hospital and blood flow restriction usage. BMC Biomed Eng. 2020;2:7.
- [CrossRef] [PubMed] [Google Scholar]
- Tourniquet palsy in upper limb; a case report. Anaesth Pain Intensive Care. 2021;25:535-8.
- [CrossRef] [Google Scholar]
- The pathophysiology of the arterial tourniquet: A review. South Afr J Anaesth Analg. 2002;8:22-9.
- [CrossRef] [Google Scholar]
- Effects of tourniquet pressure on rehabilitation outcomes in patients undergoing total knee arthroplasty. Orthop Nurs. 2013;32:217-22.
- [CrossRef] [PubMed] [Google Scholar]
- A survey of the use of tourniquet among orthopaedic surgeons in Nigeria. Niger Postgrad Med J. 2021;28:133-8.
- [CrossRef] [PubMed] [Google Scholar]
- Tourniquet injuries in hand surgery: Prevention and management in university of Calabar teaching Hospital. World J Res Rev. 2016;3:16-8.
- [Google Scholar]
- Prevention of tourniquet paralysis during the use of pneumatic tourniquets. Int J Orthop Trauma Nurs. 2011;15:57-61.
- [CrossRef] [Google Scholar]
- Tourniquet use and its complications in Norway. J Bone Joint Surg. 2006;88:1090-2.
- [CrossRef] [PubMed] [Google Scholar]








