Translate this page into:
Effect of pain neuroscience education in individuals with low back pain – A pilot feasibility study

*Corresponding author: Soundararajan Kannan, Assistant Professor, Sri Ramachandra Faculty of Physiotherapy, Sri Ramachandra Institute of Higher Education and Research (Deemed to be University), Chennai, Tamil Nadu, India. soundararajan.k@sriramachandra.edu.in; k.soundararajan1995@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Niveda MV, Kannan S, Aseer PA. Effect of pain neuroscience education in individuals with low back pain – A pilot feasibility study. Adesh Univ J Med Sci Res. 2024;6:28-31. doi: 10.25259/AUJMSR_29_2024
Abstract
Objectives
Pain neuroscience education (PNE) is an approach to managing low back pain. PNE helps individuals to understand the nature of an individual’s pain and the factors that contribute to it. It is based on the idea that chronic pain is not simply a result of tissue damage, but it is also because of complex interactions between the nervous system, the brain, and various environmental and psychological factors that contribute to pain. Understanding these interactions, which are involved through PNE, empowers individuals with spine pain to better cope and manage their pain. The broad aim of the study is to investigate the effect of pain neuroscience education in individuals with low back pain.
Material and Methods
Individuals with low back pain were recruited for this study. Aged 30 to 50 years of both genders. The participants were randomized into two groups, one group being given PNE along with standardized exercises and the other being given only standardized exercises. Visual analogue scale (VAS), range of motion of the spine, and Patient-Reported Outcomes Measurement Information System (PROMIS) were measured at baseline and end of 5th day of treatment. The data was analyzed using the SPSS 22 version, a widely used statistical software for data analysis in research studies.
Results
The statistical analysis revealed that there is a significant change in the VAS score and PROMIS 10 score (including physical and mental health subdomains) in the experimental group compared to the control group at the end of the 5th day. The range of motion didn’t show any significant differences at the end of the 5th day.
Conclusion
This study’s results support the use of PNE for spine pain helps in reducing pain ratings, limited knowledge of pain, pain catastrophizing, and fear avoidance behaviour regarding pain. This study showed that the combination of pain neuroscience education along with standardized exercises and treatment was found to be more effective than standard care treatment alone in a short-term follow-up. These findings suggest that future research should explore the long-term effects of PNE and its potential to improve patient outcomes in the field of pain management.
Keywords
Chronic pain
Exercise
Low back pain
Pain neuroscience education
INTRODUCTION
“Chronic pain” (CP) is defined by The International Association for the Study of Pain as pain that persists for more than 3 months. The pain could be due to direct injury or tissue damage. CP is also known as nociplastic pain or central sensitization, in which the nervous system becomes sensitive and shows a heightened response to non-noxious stimuli, and this is the key component in the CP experience.[1] The onset of low back pain (LBP) is from age 30, and the overall prevalence of CP among the adult Indian population is 19.3%. CP tends to be higher in females (25.2%), and the prevalence increases beyond 65 years of age.[2] The causes of chronic LBP (CLBP) are multifactorial since it involves a combination of mechanical, physical, social, and psychological factors that significantly affect the global population.[3] The term “non-specific low back pain”” (NSLBP), which refers to LBP that cannot be linked to a single identifiable cause, is frequently used to describe CLBP. The majority of the individuals do not have an underlying pathology. NSLBP often results from psychological distress or a heightened nervous system response to non-noxious stimuli that persists for a longer duration.[4] Most of the interventions focus on treating the underlying structures and soft tissues, though they were not directly involved in NSLBP. One such intervention that supports the biopsychosocial model and forms an educational strategy and therapeutic approach to treat CLBP is pain neuroscience education (PNE).
An educational strategy called PNE seeks to improve the knowledge of pain and its underlying mechanisms and also to learn self-management strategies to improve quality of life (QOL) as literature states that PNE elucidates the multidimensionality of pain experienced by the individual and also explains the neurophysiology of pain perception of the individual.[5] PNE is founded on the biopsychosocial model of pain, which views pain as a multifaceted phenomenon impacted by social, biological, and psychological elements. Individuals are taught about the neurobiology of pain through PNE, which includes how the central nervous system processes pain, what causes pain, and how stress, emotions, and beliefs affect pain.[6] There are studies in the literature which evaluated the efficacy of PNE in long-term follow-up.[7] Thus, the purpose of this study is to compare the effects of PNE and a standardized treatment at short-term follow-up to determine how they affect range of motion, physical activity, and CP.
MATERIAL AND METHODS
Individuals with NSLBP, aged between 30 and 50 years of both genders, were gathered from the outpatient department of Sri Ramachandra Hospital for this study. Individuals with any neurological disorders, sinister pathology of the spine, vertebral fracture, or cognitive impairments were excluded from the study. Informed consent was obtained before the study. Block randomization, based on a computer-generated sequence, was used to assign the individuals to two groups. Blinding was implemented for the group allocator, outcome assessor, and statistical analyzer. Fifty individuals with LBP were recruited and were randomized into experimental and control groups. The individuals in the experimental group received a session of PNE along with standardized exercises. The individuals in the control group received only standardized exercises and followed up for 5 days. PNE was delivered to the individuals through a pamphlet for 30 min in each session.
Study procedure
Fifty individuals with lower back pain were recruited, aged 30–50 years, of both genders. The participants were randomized into two groups; one group was given PNE along with standardized exercises, and the other was given only standardized exercises. PNE was conveyed to the individuals through a pamphlet in which 20–30 min of education was given about pain, the pain system, and fear avoidance behavior. After which, standardized exercise and treatment were given. Visual analog scale, range of motion of the L-spine, and patient self-reported outcomes were measured at baseline and end of 5th day of treatment as described in Figure 1.
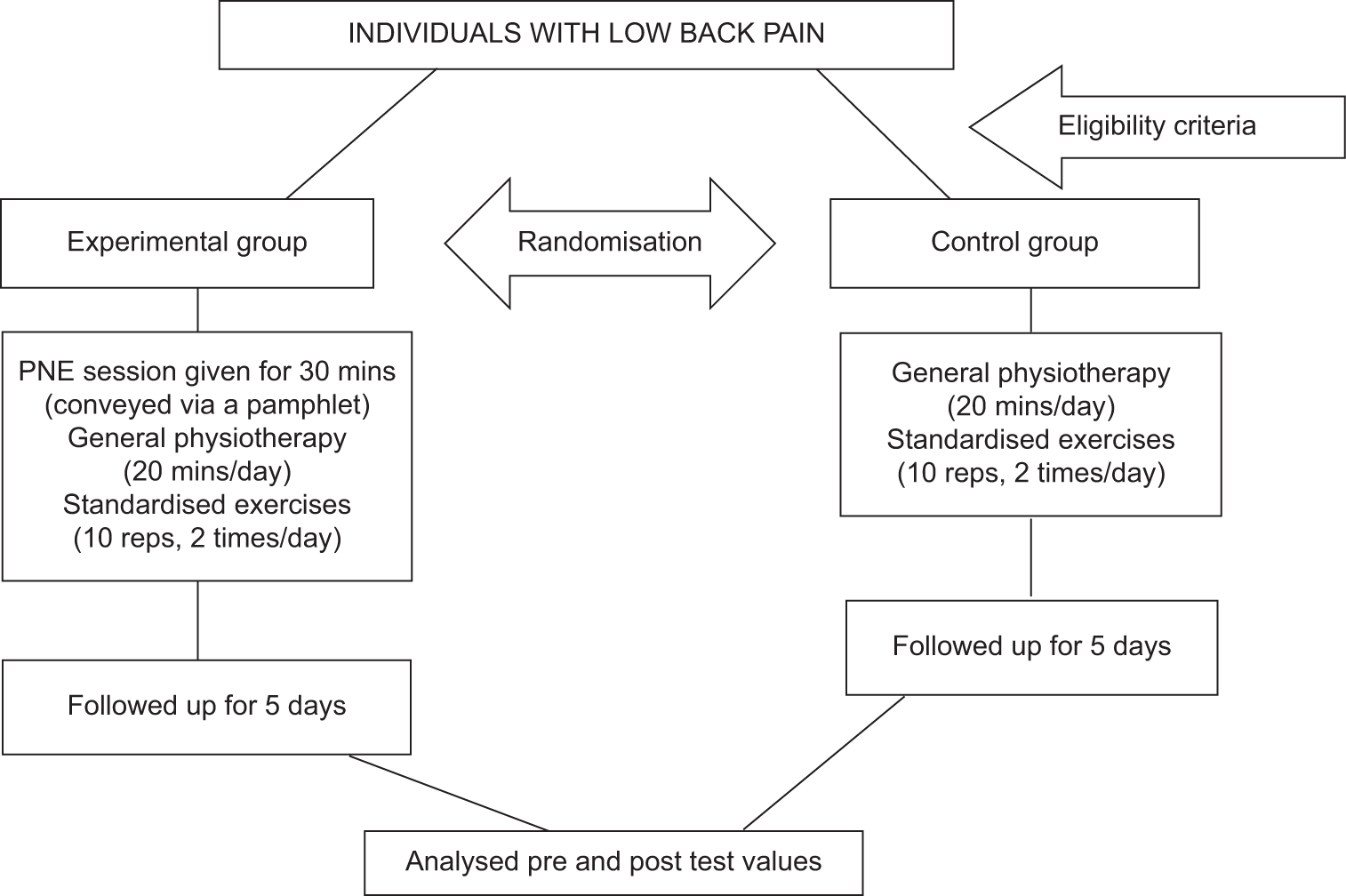
- Consolidated standards of reporting trials flowchart. PNE: Pain neuroscience education,
Statistical analysis
IBM was used for the data analysis version 23.0 of the Statistical Package for the Social Sciences statistics program. “For both continuous and categorical data, percentage analysis and descriptive statistics were applied. The Shapiro– Wilk test was used to validate the normative data. At the significance level of P > 0.01, the score was confirmed to be regularly distributed. Consequently, parametric tests were applied. The paired t-test was used to analyze repeated measures within the group. The Independent t-test was used to assess the pain between groups. When P-value is <0.01 for the statistical tests, they are deemed significant.”
RESULTS
At the end of the 5th day of the study, 50 individuals completed it, and neither group reported any adverse side effects from the therapy. There was no discernible variation in the baseline and demographic data between the two groups as described in Table 1. Within-group analysis revealed that both groups experienced improvements in range of motion, pain intensity, and patient self-reported outcomes. When comparing the variables between groups, participants in the experimental group showed more significant differences than those in the control group as described in Table 2. The pain intensity using PROMIS (Physical and Mental Health) improved in both groups, with more significant change in the experimental group. Both groups experienced a considerable change in VAS, with only the experimental group exceeding the minimal clinically important difference (MCID) and minimal detectable change (MDC) values. The post-treatment values of range of motion did not exceed the MCID value, and neither group showed significant improvement in ROM as described in Table 3. The statistical analysis revealed that there was a significant change in the VAS score and PROMIS 10 score (including physical and mental health subdomains) in the experimental group compared to the control group at the end of the 5th day. The range of motion did not show any significant differences at the end of the 5th day.
| Characteristics of the participants | Experimental group | Control group |
|---|---|---|
| Gender (male/female) | 21/29 | 23/27 |
| Age (years) | 42.85 (11.21) | 42.66 (12.25) |
| Pain duration (days) | 59.52 (68.23) | 58.14 (41.01) |
| Height (cms) | 156.33 (4.28) | 156.19 (4.50) |
| Weight (kgs) | 68.45 (6.13) | 67.57 (6.25) |
| VAS | 6.10 (1.1) | 5.50 (0.97) |
| Physical health (PROMIS 10) | 37.37 (2.8) | 39.59 (2.1) |
| Mental health (PROMIS 10) | 41.09 (5.2) | 42.05 (3.2) |
VAS: Visual analogue scale, PROMIS: Patient-reported outcomes measurement information system.
| Group | Clinical outcomes | Mean difference | SE difference | P-value | Effect size |
|---|---|---|---|---|---|
| Experimental | VAS | 3.2 | 0.4 | <0.001 | 2.2 |
| Physical health PROMIS | 9.8 | 1.4 | <0.001 | 2.7 | |
| Mental health PROMIS | 8.1 | 1.5 | <0.001 | 1.7 | |
| Control | VAS | 1.1 | 0.5 | 0.066 | 0.6 |
| Physical health PROMIS | 2.9 | 2.6 | 0.291 | 0.3 | |
| Mental health PROMIS | 3.8 | 2.3 | 0.133 | 0.5 |
SE: Standard error, VAS: Visual analogue scale, PROMIS: Patient-reported outcomes measurement information system.
| Clinical outcomes | Mean difference | SE difference | P-value | Effect size |
|---|---|---|---|---|
| VAS | 1.00 | 0.4 | 0.005 | 0.67 |
| Experimental group | 7.9 | 2.8 | 0.046 | 0.53 |
| Control group | 4.9 | 2.9 | 0.052 | 0.47 |
SE: Standard error, VAS: Visual analogue scale
DISCUSSION
One of the most prevalent musculoskeletal conditions is the chronic low back, which persists for more than 12 weeks. This study explores the importance of PNE with standardized exercises to overcome LBP in short-term follow-up. The findings of this study state that PNE improves patients’ pain along with physical and mental well-being within 5 days of follow-up. Previous studies have shown the long-term efficacy of the PNE (Louw et al., 2019).[5] This study explains how the brain reacts to pain threshold in a shorter duration. A pamphlet containing information about pain behavior, catastrophic thinking, and kinesiophobia was explained to the individuals with CLBP in one-on-one sessions, and the pain threshold and psychological distress were reduced day by day within 5 days.
Along with PNE, standardized therapeutic approaches were also added to have a better outcome. A systematic review conducted by Lepri et al.[6] in 2023 states that PNE, along with therapeutic approaches, was effective in CLBP in 3 months follow-up. The present study also proves the effectiveness of the combination of PNE with standardized approaches in short-term follow-up. In contrast, there were studies in the literature that evaluated the PNE effect in long-term follow-up. Moreover, systematic reviews conducted by Louw et al.[5] in 2019 state that there were limited randomized controlled trials (RCTs) conducted in the literature to prove the efficacy of PNE. Hence, this study fills the lacunae in the literature.
CONCLUSION
The findings of this study state that PNE benefits individuals with LBP by lowering their pain ratings, pain catastrophizing, pain ignorance, and pain-related fear avoidance behavior. This study also showed that, in a short-term follow-up, the combination of standardized exercises, PNE, and treatment proved to be more successful than the standard care treatments alone.
Ethical approval
The research/study approved by the Ethics Committee of Sri Ramachandra Institute of Higher Education and Research, number CSP/23/JUL/133/709, dated 08th September 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- The revised IASP definition of pain: Concepts, challenges, and compromises. Pain. 2020;161:1976-82.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of chronic pain among adults in India. Indian J Palliat Care. 2018;24:472-7.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic low back pain: A narrative review of recent international guidelines for diagnosis and conservative treatment. J Clin Med. 2023;12:1685.
- [CrossRef] [PubMed] [Google Scholar]
- Pain neuroscience education: Which pain neuroscience education metaphor worked best? S Afr J Physiother. 2019;75:1329.
- [CrossRef] [Google Scholar]
- Effectiveness of pain neuroscience education in patients with chronic musculoskeletal pain and central sensitization: A systematic review. Int J Environ Res Public Health. 2023;20:4098.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of pain neuroscience education program in community physiotherapy context on pain perception and psychosocial variables associated with it in elderly persons: A ranzomized controlled trial. Int J Environ Res Public Health. 2022;19:11855.
- [CrossRef] [PubMed] [Google Scholar]








