Translate this page into:
Diagnostic and intervention radiology perspective of Dieulafoy’s lesion of stomach – A case report with literature review

*Corresponding author: Rushabh Bhikhabhai Suthar, Department of Radiology, Zydus Hospitals, Ahmedabad, Gujarat, India. rushabhb84@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Suthar RB, Goswami GS. Diagnostic and intervention radiology perspective of Dieulafoy’s lesion of stomach – A case report with literature review. Adesh Univ J Med Sci Res. 2024;6:44-6. doi: 10.25259/AUJMSR_35_2023
Abstract
Dieulafoy’s lesion is a developmental vascular malformation of the gastrointestinal (GI) tract. It is a relatively uncommon cause of life-threatening GI bleeding from a dilated and tortuous submucosal artery in the absence of mucosal ulcers or erosions. With the proactive use of endoscopy-guided intervention, the mortality of the condition can be reduced. In endoscopically negative cases, imaging plays a pivotal role in diagnosing it, which can then be treated by endovascular embolization. We report a case of middle-aged female who presented with acute hematemesis. Endoscopy showed trace active oozing from a mucosa in the cardia of the stomach, in the absence of appreciable ulcer, erosion, or mass lesion. On contrast computed tomography abdomen, we detected a Dieulafoy’s lesion in the fundus of the stomach, which was then promptly embolized by endovascular route. The clinical details, imaging appearance, and treatment of this uncommon lesion are discussed here.
Keywords
Dieulafoy’s lesion
Gastrointestinal bleed
Developmental vascular malformation
INTRODUCTION
Dieulafoy’s lesion is a developmental vascular malformation of the gastrointestinal tract (GIT). It is a relatively uncommon cause of life-threatening gastrointestinal (GI) bleeding from a dilated and tortuous submucosal artery in the absence of mucosal ulcers or erosions. With the proactive use of endoscopy-guided intervention, the mortality of the condition can be reduced. In endoscopically negative cases, imaging plays a pivotal role in diagnosing it, which can then be treated by endovascular embolization.
CASE REPORT
A 39-year-old female was rushed to the emergency department with acute hematemesis and melena for 1 day. She denied a history of alcohol abuse, smoking, peptic ulcer disease, malignancy, or chronic non-steroidal anti-inflammatory drug ingestion. Clinical examination revealed a heart rate of 124/min, blood pressure 94/60 mm Hg, and hemoglobin 5.2 g%. After the initiation of hemodynamic stabilization, an emergency endoscopy was done. It showed fresh blood in the stomach with trace active oozing from a mucosa in the cardia of the stomach in the absence of appreciable ulcer, erosion, or mass lesion. Active oozing was treated with glue injection during endoscopy. An emergency computed tomography (CT) angiogram showed a tortuous tuft of dilated blood vessels in the fundus of the stomach arising from the short gastric artery (branch of splenic artery) with no appreciable active extravasation of contrast [Figure 1]. Given the location and configuration of the vessel, a diagnosis of Dieulafoy’s lesion was considered and planned for endovascular management. An angiogram of the splenic artery corroborated with CT and showed a tortuous tuft of vessels arising from short gastric arteries (branch of the splenic artery) without an early draining vein [Figure 2]. The diagnosis was confirmed, and a decision to embolize the feeding artery with 30% n-butyl cyanoacrylate (glue) was made. Through a 1.7F microcatheter, the vessel was negotiated, and embolization was performed, ensuring no collateral flow into the lesion [Figure 3]. The patient responded well, with vitals getting stabilized within an hour and resolution of melena in two days.
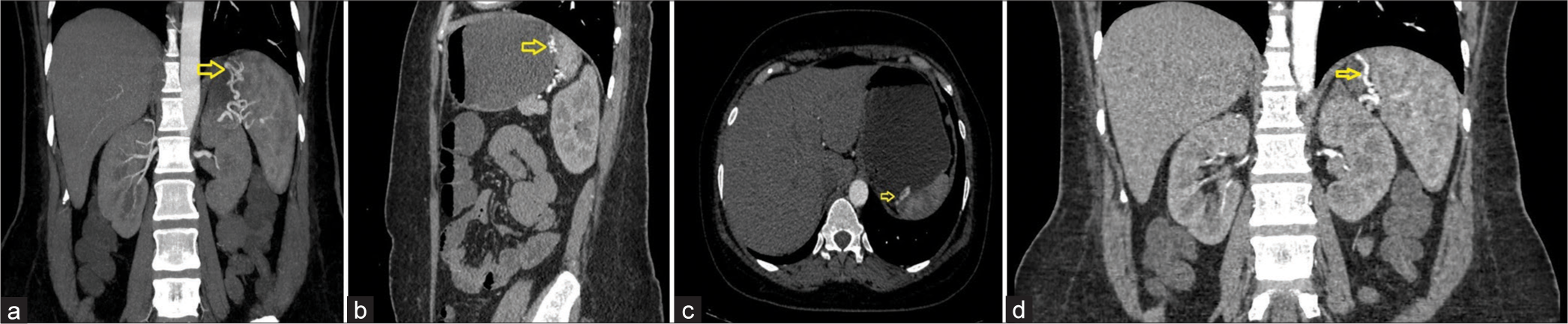
- (a-d) Computed tomography abdomen arterial phase: Yellow arrow shows a tortuous tuft of dilated vessels in the fundus of the stomach arising from the short gastric artery (branch of the splenic artery) with no active extravasation of contrast.
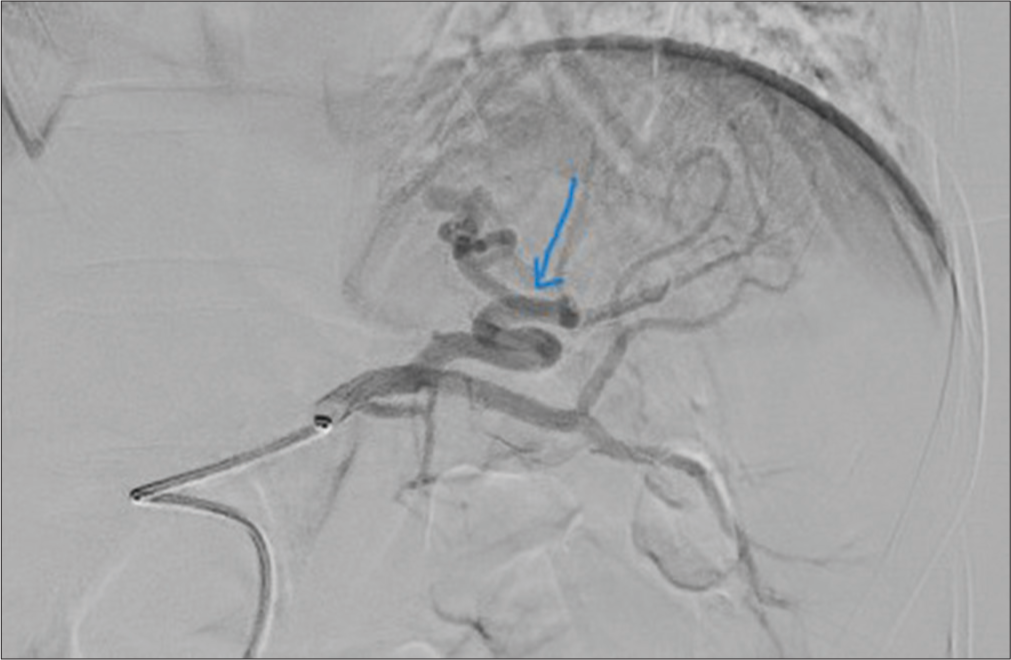
- Selective splenic artery angiogram: Blue arrow shows a tortuous tuft of dilated vessels in the fundus of the stomach arising from short gastric artery (branch of the splenic artery). No active extravasation of contrast with no early draining vein.

- Selective splenic artery angiogram: Blue arrow shows that the lesion was embolized using n-butyl cyanoacrylate (glue) with post-embolization angiogram which showed complete obliteration of the lesion.
DISCUSSION
Dieulafoy’s lesion is a developmental vascular malformation of the GIT, usually presented in the fifth decade of life. It consists of a dilated and tortuous aberrant submucosal artery protruding into mucosa from the submucosa. It erodes and eventually perforates the mucosa over time, leading to intermittent to massive GI bleeding. It is an uncommon, life-threatening cause of GI bleeding that constitutes about 1–2% of all the causes of GI bleeding and 6.5% of all causes of upper GI non-variceal bleeding.[1] The majority of the lesions arise in the stomach at the lesser curvature (within 6 cm of the gastroesophageal junction) followed by duodenum (15%), colon (5%), and rarely in the esophagus, bronchus, or anastomotic site.[2]
Accurate diagnosis and management are vital as the mortality rate due to GI bleed reduces significantly from untreated lesions (80%) to treat ones (8%).[3] Direct endoscopic visualization of Dieulafoy’s lesion is the gold-standard method for the diagnosis. Endoscopy can be challenging in certain circumstances such as active bleeding (obscuring the bleed site), in intermittent bleeds, and if the lesion occurs at “blind spot” like the fundus of the stomach. If lesions are not detected by endoscopy, a contrast CT scan can help in the diagnosis as well as management with endovascular intervention. The advantage of CT scan and digital subtraction angiography is that it can detect tortuous tuft of vessels even in the absence of active extravasation. The absence of an early draining vein in the angiogram is a vital sign to differentiate the lesion from angiodysplasia and arteriovenous malformation.
The first-line treatment modality for Dieulafoy’s lesion is endoscopic interventions such as (a) thermal-using heat probe or argon plasma coagulation; (b) regional injection of epinephrine/norepinephrine or sclerotherapy; and (c) mechanical – banding and hemoclips with a reported success rate of more than 80%.[4] Endovascular embolization is useful in failed endoscopy or lesions beyond the reach of the endoscope. Gel foam, polyvinyl alcohol particles, glue, and coils can be used for embolization[5,6] with a success rate of 60–70%. The use of glue is better in such lesions as it can percolate into distal tortuous vessels, resulting in complete occlusion of the bleeder, giving prompt response, and reducing recurrence rate.[7,8]
CONCLUSION
Dieulafoy’s lesion (DL) should be suspected in patients presenting with intermittent or severe upper GI bleed without evidence of portal hypertension, mass lesion or peptic ulcers. CT angiography has the advantage over endoscopy in DL in detecting abnormal vessels even in the absence of active bleed. Angioembolisation can be attempted in cases of failure of therapeutic endoscopy. N-butyl cyanoacrylate is a safe agent for these lesions to attain complete angioembolisation and to prevent recurrence.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- An uncommon cause of life-threatening gastrointestinal bleeding: 2 synchronous Dieulafoy lesions. J Pediatr Surg. 2009;44:441-3.
- [CrossRef] [PubMed] [Google Scholar]
- Gastrointestinal bleeding from Dieulafoy's lesion: Clinical presentation, endoscopic findings, and endoscopic therapy. World J Gastrointest Endosc. 2015;7:295-307.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes in Dieulafoy's lesion: A 10-year clinical review. Dig Dis Sci. 2015;60:2097-103.
- [CrossRef] [PubMed] [Google Scholar]
- Dieulafoy's lesion of the duodenum: A comparative review of 37 cases. BMJ Case Rep. 2018;2018:bcr2017223246.
- [CrossRef] [PubMed] [Google Scholar]
- Dieulafoy lesions: A review of 6 years of experience at a tertiary referral center. Am J Gastroenterol. 2001;96:1688-94.
- [CrossRef] [PubMed] [Google Scholar]
- Dieulafoy disease: Arteriographic findings and treatment. Radiology. 1990;174:937-41.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic management of Dieulafoy's lesion using Isoamyl-2-cyanoacrylate. World J Gastrointest Endosc. 2013;5:417-9.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic management of Dieulafoy lesions of the stomach: A case study of 26 patients. Endoscopy. 1997;29:834-9.
- [CrossRef] [PubMed] [Google Scholar]







