Translate this page into:
Comparison between interlocking nailing and plate fixation of tibial diaphyseal fractures in adults

*Corresponding author: Joseph Effiong Asuquo, Department of Orthopaedics and Traumatology, University of Calabar, Calabar, Nigeria. itansuq@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Ofoegbu JI, Lasebikan OA, Asuquo JE, Mbalewe C, Ihezia C, Akpet OE, et al. Comparison between interlocking nailing and plate fixation of tibial diaphyseal fractures in adults. Adesh Univ J Med Sci Res. 2024;6:38-43. doi: 10.25259/AUJMSR_44_2023
Abstract
Objectives
Tibial diaphyseal fractures (TDFs) often result from high-energy forces and occur mostly among young adults. The mainstay of the treatment is operative fixation. We compare the outcome between locked intramedullary nailing (IMN) and plating of TDFs.
Material and Methods
This was a prospective comparative study conducted over an 18-month duration. Patients were selected in a randomized fashion and data were collected with a pro forma. Clinical, radiographic, and functional results were evaluated using Johner–Wruh’s criteria. Data were analyzed using the Statistical Package for the Social Sciences version 21. Significant statistical inference was <0.05.
Results
Ninety-six patients with hundred TDFs were recruited, and 10 patients were lost to follow-up leaving a total of 90 TDFs in 86 patients (45 fractures in each group). Locked IMN had an average duration of surgery of 115.16 ± 16.7 min, while it was 95.87 ± 14.74 min for plate fixation. The average duration of hospital stay was 18.12 ± 10.78 and 21.4 ± 12.94 days for plate fixation and locked IMN, respectively. At 18 weeks, the bone union had been achieved in 97.8% of locked IMN group and 91.1% of plate fixation group. There was a statistically significant wound infection rate of 4.4% in the locked IMN group and 17.8% in the plating group. The overall limb length discrepancy was 17.8% in the locked IMN group and 8.9% in the plating group.
Conclusion
Locked IMN technique is marginally superior to plate fixation. They can be used for the treatment of tibial shaft fractures.
Keywords
Locked intramedullary nail
Plate osteosynthesis
Open tibial fractures
Closed tibial fractures
INTRODUCTION
The tibia is the most common site for long bone fractures and open fractures in adults as seen in Western Nigeria.[1,2] This is a result of the subcutaneous nature of the anteromedial surface of the tibia.[3] This fracture poses a huge burden to the individual involved, the family and the society at large.[1,2] They account for approximately 77,000 hospitalizations, 569,000 hospital days (average length of stay of 7.4 days), and 825,000 office visits per annum.[3] The increasing incidence of tibial shaft fracture in young adult is a result of high-speed lifestyles with motor vehicles, snowmobiles and motorcycles, as well as extreme sports. However, in the elderly, simple falls cause most of the tibial shaft fractures. In addition, complex fracture configurations are frequently seen in older patients due to the osteoporotic nature of the bone.[4] Road traffic injuries account for the majority of the cases.[4] Tibial fractures can be closed or open. Closed tibial fractures usually have a simpler fracture pattern with less severe soft-tissue injury than open tibial shaft fractures.[3] The modality of treatment could be conservative or operative. Conservative treatment can be undertaken using casts or functional braces, while operative treatment entails closed or open reduction and internal fixation with plates, external fixators, and intramedullary nail (IMN).[3] Several studies have been done comparing the treatment outcome and complications following fixation of tibial diaphysis fractures by plate fixation and IMN.[5-7] A study by Huang et al.[5] showed that the operation time was 84.0 ± 9.2 min for locked IMN and 69.0 ± 8.4 min for plate fixation.[5] There is a significant statistical difference in operation times (P < 0.05) from his study. Other authors found the mean operation time to be the same in both.[6,7] Some studies showed that the mean union time was 3.3 months[5,7] with IMN while another showed that it took 5 months.[6] In the case of plate fixation, two studies revealed a bone union time of 3.5 months[6,7] while another said that it takes 3.1 months.[5] Limb length discrepancy was seen to occur with IMN only,[5-7] and other complications that could follow any treatment protocol include infection (superficial or deep), mal-alignment, delayed union, non-union, and knee pain.[6,7] However, a study reported that plate fixation has fewer complications than IMN.[5]
On account of the controversies and lack of adequate randomized controlled trials comparing the efficacy of these two methods of tibial diaphyseal fracture (TDF) fixation in our environment, it is therefore necessary to undertake this study. We compare the outcome of IMN and plate osteosynthesis of tibial fractures.
MATERIAL AND METHODS
This is a prospective, comparative study that was carried out in a tertiary hospital in Southern Nigeria. It was conducted from May 1st, 2016, to October, 31st, 2017. The first 12 months were for patients’ recruitment, treatment, and follow-up while the last 6 months were for treatment and follow-up of patients recruited for the study in the 7th–12th month of the study.
Ninety TDFs in 86 patients were studied and analyzed. Patients who met the inclusion criteria were 18 years and above with closed tibial shaft fractures or open tibial shaft fractures; Gustilo and Anderson type I and II only (they were evenly distributed across both groups), occurring within 4 weeks were recruited for the study. Treatment options for the patients with TDF presenting at the emergency unit or orthopedic clinics were selected by randomization.
Data were collected using a pro forma. This includes demographic data, procedure data, the operating time (in minutes), duration of hospital stay (in days), time for bone union (in weeks), and possible complications from both operative measures. Informed consent was obtained from the patients.
Data analysis
Statistical analysis was carried out using the Statistical Package for the Social Sciences (version 21; IBM Corp., Armonk, NY, USA). The results were presented in tables and, where appropriate in bar or pie charts. Fisher’s exact and Chi-square tests were used to test for the level of significance of variables in terms of association. The confidence interval was calculated at 95% level and significance was at 5% probability level (P < 0.05).
Ethical clearance was obtained from the Institutional Ethical and Research Committee Health Research and Ethics Committee (HREC) 2419.
RESULTS
Using the Johner–Wruh’s criteria, good to excellent outcome was achieved in more patients (32; 71.1%) in the IMN group than the plating group (28; 72.2%) as shown in Table 1. The difference between the 2 groups was not statistically significant (x2 = 1.224; P = 0.522).
| Johner-Wruh’s outcome | Group | |
|---|---|---|
| Locked IM nailing n(%) | Plating n(%) | |
| Excellent | 31 (68.9) | 25 (55.5) |
| Good | 1 (2.2) | 3 (6.7) |
| Fair | 6 (13.3) | 7 (15.6) |
| Poor | 7 (15.6) | 10 (22.2) |
| Total | 45 (100.0) | 45 (100.0) |
IM: Intramedullary
The average duration of surgery was 115.16 ± 16.7 min for locked IMN and 95.87 ± 14.74 min for plate fixation [Table 2].
| Duration of surgery (mins) | Group | |
|---|---|---|
| Locked IM nailing n (%) | Plating n (%) | |
| <60 | 0 (0.0) | 0 (0.0) |
| 61 – 70 | 0 ( 0.0 ) | 1 (2.3) |
| 71 – 80 | 0 ( 0.0 ) | 4 (8.9) |
| 81 – 90 | 3 (6.7) | 10 (22.2) |
| 91 – 100 | 6 (13.3) | 11 (24.4) |
| 101 – 110 | 8 (17.8) | 11 (24.4) |
| 111 – 120 | 10 (22.2) | 5 (11.1) |
| 121 – 130 | 11 (24.4) | 2 (4.4) |
| 131 – 140 | 4 (8.9) | 0 ( 0.0 ) |
| >141 | 3 (6.7) | 1 (2.3) |
IM: Intramedullary
The average duration of admission was 11–20 days for 20 (46.5%) patients in the locked IMN group while only 19 (44.2%) of patients in the plate fixation group were on admission for the same period [Table 3]. When both groups were compared, it was not statistically significant (P = 0.572).
| Days on admission | Group | |
|---|---|---|
| Locked IM nailing n (%) | Plating n (%) | |
| 0 – 10 | 8 (18.6) | 3 (7.0) |
| 11 – 20 | 20 (46.5) | 19 (44.2) |
| 21 – 30 | 10 (23.3) | 14 (32.5) |
| 31 – 40 | 3 (7.0) | 3 (7.0) |
| 41 – 50 | 1 (2.3) | 2 (4.7) |
| 51 – 60 | 0 ( 0.0 ) | 1 (2.3) |
| 61 – 70 | 1 (2.3) | 0 (0.0) |
| 71& above | 0 ( 0.0 ) | 1 (3.8) |
IM: Intramedullary
At 6 weeks, bridging callus was noted in 40 (88.9%) fractures of the locked IMN group and 36 (80%) fractures of the plate fixation group. At 18 weeks, 44 (97.8%) fractures in the IMN group had radiological union while 41 (91.1%) had radiological union in the plating group [Table 4]. When the time of radiological bone union in both groups was subjected to statistical tests of significance, it was not significant (Fisher’s exact test = 0.180). This percentage of patients in both groups commenced full weight bearing at 18 weeks.
| Time of callus formation | Group | Fisher’s exact test | |
|---|---|---|---|
| Locked IM nailing n (%) | Plating n (%) | ||
| Callus in the fracture site at 6 wks | |||
| Yes | 40 (88.9) | 36 (80.0) | 0.192 |
| No | 5 (11.1) | 9 (20.0) | |
| Bridging callus in the fracture at 12 wks | |||
| Yes | 43 (95.6) | 38 (84.4) | 0.079 |
| No | 2 (4.4) | 7 (15.6) | |
| Bridging callus in the fracture at 18 wks | |||
| Yes | 44 (97.8) | 41 (91.1) | 0.180 |
| No | 1 (2.2) | 4 (8.9) | |
| Bridging callus in the fracture at 24 wks | |||
| Yes | 44 (97.8) | 41 (91.1) | 0.180 |
| No | 1 (2.2) | 4 (8.9) | |
IM: Intramedullary, IMN: Intramedullary nailing
Shortening or limb length discrepancy was identified to be relatively more in the locked IMN group 8 (17.8%) than the plate fixation group 4 (8.9%). When both groups were compared, it was not statistically significant (P = 0.176).
An overall wound infection rate of 17.8% was reported in the plate fixation group and 4.4% for the locked IMN group. Some patients had wound infections at different follow-up periods. They were majorly superficial infections except for three cases that were deep. The organisms cultured from the wounds were Staphylococcus aureus in seven cases, Pseudomonas aeruginosa in a case, and no organisms in the two remaining cases. These were treated with wound dressing and antibiotic therapy. It was statistically significant when both groups were compared (Fisher’s exact = 0.045).
The majority of the fractures (95.3%) were unilateral with a right-to-left side ratio of 1.3:1. Thirty-four (37.8%) of the fractures were open. Using Gustilo–Anderson classification, Type I accounted for 35.3% while Type II accounted for 64.7% [Table 5].
| Fracture type | Locked IM nailing n(%) | Plating n(%) |
|---|---|---|
| Open | 17 (30.8) | 17 (31.8) |
| Closed | 28 (69.2) | 28 (68.2) |
| Total | 45 (100.0) | 45 (100.0) |
IM: Intramedullary
The most common cause of fracture is motor vehicular accidents, accounting for 54.4%, followed by motor cycle/tricycle (21.1%) as shown in Figure 1.
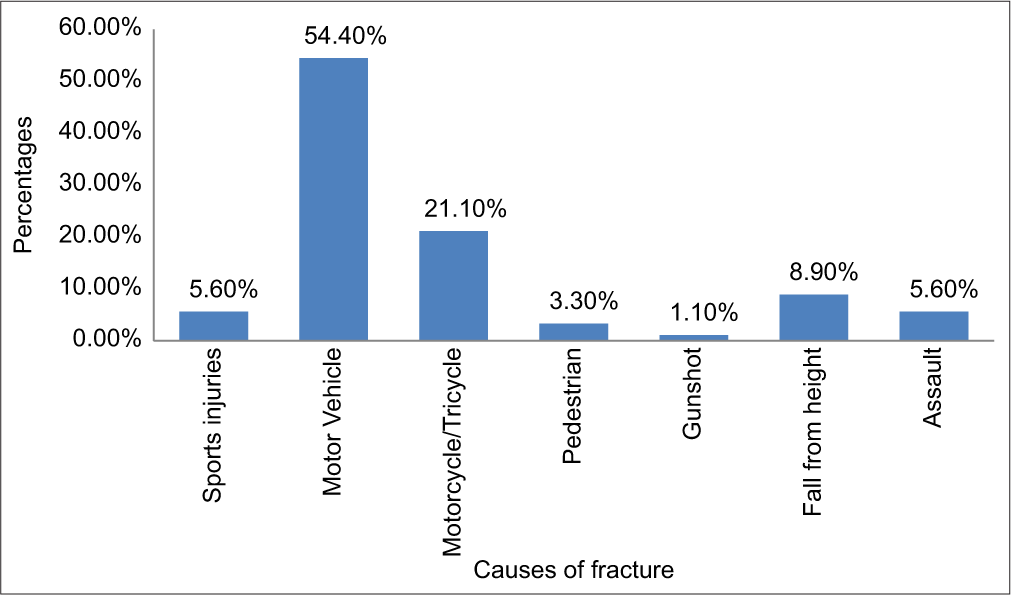
- Mechanism of injury.
The mean age was 37.6 ± 14.6 years with a range of 18–83 years and a male-to-female ratio of 2.6:1.
Figures 2-5 shows radiographs selected from each of the groups for illustrations.

- X-ray of a 24-year-old male with Gustilo–Anderson II segmental tibial fracture to be fixed with SIGN intramedullary nailing. SIGN: Surgical implant generation network

- Post-fixation X-ray with intramedullary nailing.

- X-ray of a closed mal-united tibial shaft fracture in a 44-year-old female.

- Post-plate fixation radiograph.
DISCUSSION
The treatment of tibial shaft fractures has shifted toward locked IMN due to the associated advantages of less bone stripping, minimal tissue damage, and minimally invasive in some instances. This study will show that the outcomes between plate osteosynthesis and locked IMN are comparable. The patients in both groups were evaluated clinically, radiologically, and functionally based on the Johner–Wruh’s criteria. We obtained a good to excellent outcome in a greater percentage of patients in both groups. This was similar to the outcome reported by a study even though the authors’ finding was in locked IMN.[8]
In our study, the mean operation time was relatively longer in the IMN group than the plating group. This was similar to that reported by a study[5] but other authors found the mean operation time to be the same in both groups.[6,7] An Indian study reported longer operation time for the plating group.[9] The reason for this in our environment could be due to the lack of image guidance, steep learning curve for IMN without image guidance, poor instrumentation, and delay in nurses getting the right instrumentation. Our study reveals a relatively longer duration of admission in both groups. This finding differs from that reported by two studies where there were relatively short and very short hospital stays for locked IMN and plate fixation.[9,10] This difference may be due to the variability in the pattern and severity of associated injuries in the patients. In addition, patients in our environment pay out of pocket for their treatment and may have financial constraints, which can prolong their stay in the hospital. Moreover, in developed climes, hospital aftercare is continued at home by general practitioners or peripheral centers, which encourages early discharge postoperatively.
In our study, a greater percentage of the patients had radiological union in both groups at 18 weeks. This finding was corroborated by studies from different continents. A Brazilian study reported 20 weeks and 16 weeks, while a Chinese study reported 13.2 weeks and 12.4 weeks and an American study reported 20 weeks and 13 weeks for IMN and Plating groups, respectively.[7,10,11] This union time in our study corresponds to the time of full weight bearing in both groups.
The limb length discrepancies that were reported in this study were all in the form of shortening, with a prevalence of 17.8% in the locked IMN group. This was higher compared to the prevalence of 7.9% and 5.0% reported by other studies.[12,13] We reported a prevalence of 8.9% in the plating group, while a Scandinavian study reported 0% prevalence.[14] The higher rate in this study is probably because they studied only closed tibial shaft fractures. Furthermore, locked IMN gives relative stability as against plate fixation that gives rigid stability. This could make fractures fixed by locked IMN prone to shortening.
Our study reveals a higher infection rate in the plating group than in the locked IMN group. This was similar to that reported by other studies, even though they had no infection in the IMN group.[9,10] This could be due to the fact that their fractures were close fractures, which were fixed by closed IMN method, probably with image guidance, unlike in this study where both open and closed fractures were fixed. The rate of wound infection is directly proportional to the grade and severity of the injury.[12]
In our study, road traffic injuries were the most common cause of approximately 80% of the fractures. This was similar to that reported by other West African studies.[1,2,4] This is probably because almost everyone uses the road and the use of cars and buses is the most common means of intracity and intercity transportation in our environment.
Our study reveals a male preponderance and a young age group constituting a greater percentage of the patients. These findings have been reported by other studies within and outside Africa.[1,2,5] This preponderance is probably because this is the active age group in the society with preference for high-speed lifestyles with motor vehicles, snowmobiles and motorcycles, as well as extreme sports.[4]
The strength of the study is in the randomization of both open and closed fractures, which increases its inclusiveness. The sample size is small to make inferential conclusions. However, more studies can be carried with large sample sizes.
Recommendations
It is therefore recommended that based on the findings, locked IMN technique and plate fixation can be used for the treatment of both open and closed tibial shaft fractures in adults.
CONCLUSION
Operative treatments of tibial shaft fractures by locked IMN and plate fixation have shown comparative results.
Fixation by locked IMN is marginally superior to plate fixation in terms of a lower infection rate as well as excellent outcome and fewer poor outcomes using the Johner–Wruh’s criteria.
Ethical approval
The research/study approved by the Institutional Review Board at Federal Medical Centre Owerri, number 2419, dated 01st June, 2017.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Management of tibial shaft fractures using locked Intramedullary nails: Our Experience from Jos, North central, Nigeria. IOSR J Dent Med Sci. 2015;14:33-6.
- [Google Scholar]
- Changing trends in the pattern of tibial fractures in Nigeria: A review of 70 cases. J Orthop. 2008;5:21-8.
- [Google Scholar]
- Epidemiology of open tibial fractures in a Teaching Hospital. Port Harcourt Med J. 2007;1:156-60.
- [CrossRef] [Google Scholar]
- Comparison of LCP and locked intramedullary nailing fixation in treatment of tibial diaphysis fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2007;21:1167-70.
- [Google Scholar]
- A comparison between locked intramedullary nailing and plate-screw fixation in the treatment of tibial diaphysis fractures. Acta Orthop Trumatol Turc. 2004;38:104-9.
- [Google Scholar]
- A comparative study between intramedullary interlocking nail and plate-screw fixation in the treatment of tibial shaft fractures. Zhongguo GU Shang. 2008;21:216-3.
- [Google Scholar]
- Outcome of regular nailing in fracture of proximal third tibial shaft. Int J Orthop Sci. 2016;2:142-8.
- [Google Scholar]
- Intramedullary nailing versus proximal plating in the management of closed extra-articular proximal tibial fracture: A randomized controlled trial. J Orthop Trauma. 2015;23:485-92.
- [Google Scholar]
- Closed fractures of the tibial shaft. A meta-analysis of three methods of treatment. J Bone Joint Surg Am. 1998;80:174-83.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative multicenter study of treatment of multi-fragmented tibial diaphyseal fractures with non-reamed interlocking nails and with bridging plates. Clinics. 2006;61:333-8.
- [CrossRef] [PubMed] [Google Scholar]
- The treatment of closed, unstable tibial shaft fractures with unreamed interlocking nails. Clin Orthop Relat Res. 1995;315:48-55.
- [CrossRef] [Google Scholar]
- Unstable fractures of the tibia treated with a reamed intramedullary interlocking nail. Clin Orthop Relat Res. 1995;315:56-63.
- [CrossRef] [Google Scholar]
- Tibial fractures treated by AO compression osteosynthesis. Experiences from a five year material. Acta Orthop Scand. ;140(Suppl 1972):1-104.
- [CrossRef] [PubMed] [Google Scholar]







