Translate this page into:
An unusual presentation of large colloid goiter – A case report

*Corresponding author: Grace Budhiraja, Department of ENT, Adesh Institute of Medical Sciences and Research, B-6, AIMSR, Bathinda -Barnala Road, NH7, Bathinda - 151 001, Punjab, India. dr.gracebudhiraja148@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Budhiraja G, Dhingra HS, Guram D, Goyal S, Bharti P. An unusual presentation of large colloid goiter – A case report. Adesh Univ J Med Sci Res 2020;2(1):64-6.
Abstract
Benign nodular goiter is a frequently encountered endocrine disorder during routine clinical practice, especially in countries like India where iodine deficiency is endemic. Here, we present the case history of a 55-year- old male who presented with a large thyroid swelling. Investigations revealed it to be colloid goiter. The right hemithyroidectomy under general anesthesia was done. Post-operative period was uneventful. Hence, in this article, we discuss management of thyroid nodules which depend on assessment of thyroid function, fine-needle aspiration cytology, and imaging. For such nodules, surgery is the most common method of treatment.
Keywords
Multinodular goiter
colloid goiter
hemithyroidectomy
INTRODUCTION
Benign nodular goiter is one of the most common endocrine disorders, especially in countries like India, where iodine deficiency is endemic.[1] Goiter is an enlargement of the thyroid gland irrespective of its pathology caused by compensatory hyperplasia and hypertrophy of follicular epithelium. Nodular goiter is rarely seen before middle age and is more common in females.[2] We are presenting a case of large colloid goiter. Nowadays with the advent of daily use of iodized salt and increased awareness about the deficiency of iodine, the occurrence of large colloid goiters has become a rarity. Hence, when in clinical practice, such a huge thyroid nodule is encountered that too which is unilateral that it becomes an interesting case mandating reporting.
CASE DESCRIPTION
A 55-year-old male presented to our outpatient Department of Otolaryngology and Head and Neck Surgery, Adesh University, Bathinda with large swelling over the anterior part of neck for past 2 years. Clinical examination revealed smooth lobulated solid mass approximately 10 × 10 × 10 cm3 in size extending from below the chin to the suprasternal notch [Figure 1].

- Pre-operative lesion from the left lateral position.
Swelling moved with deglutition, and there were no dilated vessels over the swelling. No enlarged lymph nodes in the neck were palpated.
Thyroid function test (TFT), ultrasonography (USG), fine-needle aspiration cytology (FNAC), and computerized tomography (CT) were advised. Although TFT was normal, USG showed features of colloid goiter, FNAC showed many colloidophages and few groups of benign follicular epithelial cells with background showing abundant thin colloid and hemorrhage. CT scan showed a large cystic lesion with heterogeneously enhancing soft tissue in it in the right lobe of thyroid along with conglomerate lymph nodal mass along the right external jugular vein [Figure 2].

- Pre-operative lesion from the right lateral position.
All other hematological and biochemical tests were within normal limits. On the basis of above findings, surgery, namely, hemithyroidectomy was planned under general anesthesia. Horizontal skin incision was given extending from one anterior border of sternocleidomastoid (SCM) to other anterior borders of SCM about two finger breath above suprasternal notch. Subplatysmal flaps were raised superiorly (upper) up to thyroid notch and inferiorly (lower) to clavicle. Midline vertical incision was made in fascia separating the two sternohyoid muscles and separated from the thyroid gland. Gentle finger dissection was used to free the swelling from the surrounding soft tissues. Thyroid capsule identified, dissected, and subcapsular dissection of swelling started. Inferior thyroid veins which formed venous plexus in front of trachea were identified and ligated. Branches of inferior thyroid artery were ligated medially preserving blood supply to parathyroids then dissection of superior thyroid pedicle and the upper pole was done and vessels ligated, preserving the parathyroids, isthmus was separated from trachea and clamped, wound irrigation was done, drain kept and closure of wound done in layers [Figure 3].

- Specimen after thyroidectomy.
The patient was observed in ward after keeping the patient in post-operative recovery room for 2 h. There were no features of hypocalcemia and hoarseness of voice postopertaively. The patient was kept in ward for 5 days during which period daily dressings were done in minor operation theater (OT). Sutures were removed on 10th post-operative day. The specimen was sent for histopathological examination that revealed colloid goiter [Figure 4].
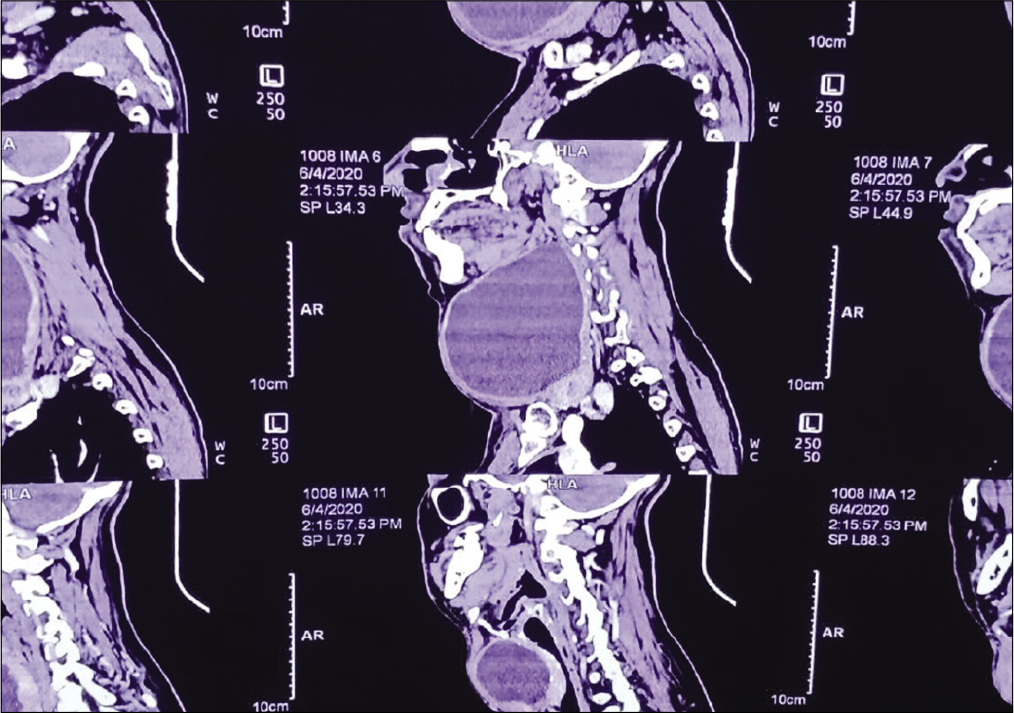
- Contrast-enhanced computed tomography neck.
DISCUSSION
When diffuse enlargement of the thyroid occurs in the absence of nodules and hyperthyroidism, it is referred to as a diffuse non-toxic goiter also called “simple goiter” due to the absence of nodules, or “colloid goiter” due to the presence of uniform follicles that are filled with colloid. Diffuse goiter is most commonly caused by iodine deficiency and is termed “endemic goiter” when it affects >5% of the population in a given geographic area.[1]
The prevalence of goiter, diffuse, and nodular is dependent on the status of iodine intake of the population. In countries with a previous deficiency corrected by universal salt iodination, elderly subjects may have a prevalence of approximately 10%. This can be attributed to lack of nutritional iodine in early adult life, as longstanding endemic goiters usually do not regress with iodine supplementation.[2]
Etiology of Multinodular goiter, also called nodular hyperplasia, involves irregular enlargement of thyroid gland due to repeated episodes of hyperplasia and involution (degeneration) of simple goiter. Thyroid gland often weighs 100 g or more and may resemble a neoplasm, particularly if a single firm dominant nodule is present. Nodules are clonal or polyclonal and are due to heterogeneous responses of follicular epithelium to TSH. Exophthalmos of Graves’ disease is not present.
Indications for treatment of non-toxic multinodular goiter are compression of the trachea or esophagus, venous-outflow obstruction, growth of the goiter, neck discomfort, and cosmetic issues.[3]
Therapeutic options include surgery, thyroxine therapy, and radioiodine therapy
In surgery, though for non-toxic multinodular goiter, bilateral subtotal thyroidectomy is standard therapy for patients, if only one lobe is enlarged, unilateral lobectomy and isthmectomy may suffice. The identification of recurrent laryngeal nerve (RLN) and parathyroid glands is accepted by most authors. Special surgical techniques, for example, capsular dissection technique and neuromonitoring, may further improve the results of surgery and avoid complications.[4]
Surgical morbidity may occur such as post-operative tracheal obstruction due to hemorrhage or tracheomalacia, injury to recurrent laryngeal nerve (1–2% of cases when surgeon is experienced), hypoparathyroidism (0.5–5% of cases), and voice changes due to superior-laryngeal-nerve damage and hypothyroidism.[5]
There is no evidence that long-term thyroxine therapy alters the natural history of multinodular goiter.
Management of thyroid nodules depends on the assessment of thyroid functions, ultrasonography, fine-needle aspiration cytology, and imaging.[3] Surgery is the common method of treatment whenever possible while other options include radioactive iodine.[6]
Surgery of thyroid is undertaken to exclude any malignancy or if there is benign thyroid disease which gives rise to dysphagia or stridor following compression of esophagus or trachea and for the cosmetic purpose.[7]
In our case, we did right-sided hemithyroidectomy and patient is not having any symptoms that were present before surgery.
CONCLUSION
The majority of thyroid nodules are benign, as in this case. However, if the thyroid nodule is very big, it produces compressive symptoms such as dysphagia or stridor. Surgery is the effective treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Genetic and environmental factors in the aetiology of simple goiter. Ann Med. 2000;32:153-6.
- [CrossRef] [PubMed] [Google Scholar]
- Approach to and treatment of goiters. Med Clin. 2012;96:351-68.
- [CrossRef] [PubMed] [Google Scholar]
- The Thyroid Gland: Function Tests and Imaging, Scott-brown's. In: 7th ed. Vol 1A. London: Hodder Arnold; 2008. p. :327-37. Ch. 27
- [CrossRef] [Google Scholar]
- The role of radioiodine therapy in benign nodular goitre. Best Pract Res Clin Endocrinol Metab. 2014;28:619-31.
- [CrossRef] [PubMed] [Google Scholar]
- Thyroid volume measured by ultrasonography and CT. Acta Radiol. 2002;43:269-74.
- [CrossRef] [PubMed] [Google Scholar]
- Environmental natural goitrogens In: Peter F, Wiersinga WM, Hostalek U, eds. The Thyroid and Environment. New York: Schattauer; 2000. p. :69-78.
- [Google Scholar]
- Evaluation and treatment of sporadic nontoxic goiter-some answers and more questions. J Clin Endocrinol Metab. 2001;86:994-7.
- [CrossRef] [PubMed] [Google Scholar]







