Translate this page into:
Incidence of fungal keratitis in Libya: An epidemiological study

*Corresponding author: Ahmed Atia, Department of Anesthesia and Intensive Care, University of Tripoli, Tripoli, Libya. ah.atia@uot.edu.ly
-
Received: ,
Accepted: ,
How to cite this article: Atia A, Ashour A, Alfaigh H. Incidence of fungal keratitis in Libya: An epidemiological study. Adesh Univ J Med Sci Res 2021;3:96-9.
Abstract
Objectives:
The aim of this study was to assess the occurrence of eye fungal infection among patients attending the eye hospital in Tripoli city, Libya.
Materials and Methods:
Seventy-one patients with ocular fungal infections were subjected to clinical and microbiological investigations. They were selected from patients attending the Tripoli Eye Hospital. The specimens of the external ocular infections were collected using sterile swab and inoculated to different culture media. Data were presented as count and percentages.
Results:
The current findings showed that Aspergillus was the most common causative agent, being responsible for 91.54% of the all cases, followed by Candida albicans (8.46%).
Conclusion:
Occurrence of fungal keratitis gradually increased in the years after 2009, especially after 2013. Knowledge of the pathological course and clinical features of fungal keratitis will undoubtedly bead in early diagnosis and treatment, with reduction in ocular morbidity.
Keywords
Eye
Infection
Dermatophytic
Clinic
INTRODUCTION
Ocular fungal infections (ophthalmic mycosis) are significant causes of morbidity and blindness (or even life-threatening infections) worldwide.[1] Among corneal diseases, the major cause of blindness is microbial keratitis.[2] Ocular ulceration and trauma are major causes of corneal blindness, often sub-related, but may be responsible for 1.5–2.0 million new cases of monocular blindness per year. Furthermore, the incidence of corneal diseases varies from nation to others and also from population to population.[1] In developed countries (North America, West Europe, and Australia), a high proportion of bacterial ulcers has been identified, and the highest proportion of corneal infections in Libya is related to fungi.[3]
A major cause of microbial keratitis is fungal keratitis.[2] An increase in its occurrence has been conveyed in recent years, but in terms of diagnosis and treatment, the disease is still a challenge.[4-7] Among the prevalent causes of fungal keratitis worldwide are Aspergillus and Fusarium. Aspergillus has the worst prognosis in general, but it shows a positive response to antifungal drugs.[3,8]
Medical suspicion is the main factor in the diagnosis of mycotic keratitis.[9] The clinical presumption of a microbial keratitis agent may be based on clinical and epidemiological evidence, and clinical suspicion may be useful in directing antimicrobial therapy and early therapy.[10] Reports on etiological and epidemiological facts of fungal keratitis patients provide valuable insights into how this possibly overwhelming corneal disease is understood, and the consequence of this condition can be enhanced by a proper understanding of the agent and host factors involved in these infectious processes.[11,12]
If untreated, fungal keratitis may result in complications such as hypopyon formation and even sight-threatening endophthalmitis. Fungal keratitis, such as fungal scleritis, can also lead to local complications. In certain countries, it is a significant cause of mono-ocular blindness.[13,14] There is no research on the actual prevalence and occurrence of fungal keratitis with its associated morbidity in Libya. Hence, the objectives of this study were to determine the occurrence of eye fungal infection among patients attending the eye hospital in Tripoli city, Libya.
MATERIALS AND METHODS
The study was conducted with the approval of the committee of Faculty of Medical Technology, The University of Tripoli, Libya (RCC-MedTech-01), and was designed as a retrospective chart review. Archives of all identified cases of fungal keratitis at the eye hospital of Tripoli from January 2009 to June 2018 were studied. Patients were diagnosed based on the International Disease Classification and by the microbiology laboratory database of the hospital. Inclusion criteria were positive culture for fungus based on their macroscopic and microscopic features. Patients were excluded if they had ocular infection with other organisms than fungi.
The collected data included patient demographics, source of sample, department of the hospital, and laboratory results. All patients were involved for the analysis of occurrence, risk aspects, and laboratory outcomes. The obtained data were gathered in Microsoft Excel sheath and descriptively presented as counts and percentages.
RESULTS
Seventy-one cases of fungal keratitis were identified during the study period. Overall, 52.2% were female. The most identified causative organism in the current study was Aspergillus 91.5% followed by Candida albicans 8.5% [Table 1].
| Fungal isolate | Number | Percentage |
|---|---|---|
| Aspergillus | 65 | 91.5 |
| Candida albicans | 6 | 8.5 |
The extent of the fungal infections during the years from 2009 to 2018 and the relationships between them, and the source of collection either floor, OPD, or casualty are shown in Figures 1 and 2. Most of the case samples were collected form floor constituted 84.5% followed by OPD and causality (11.2% and 4.2%, respectively).
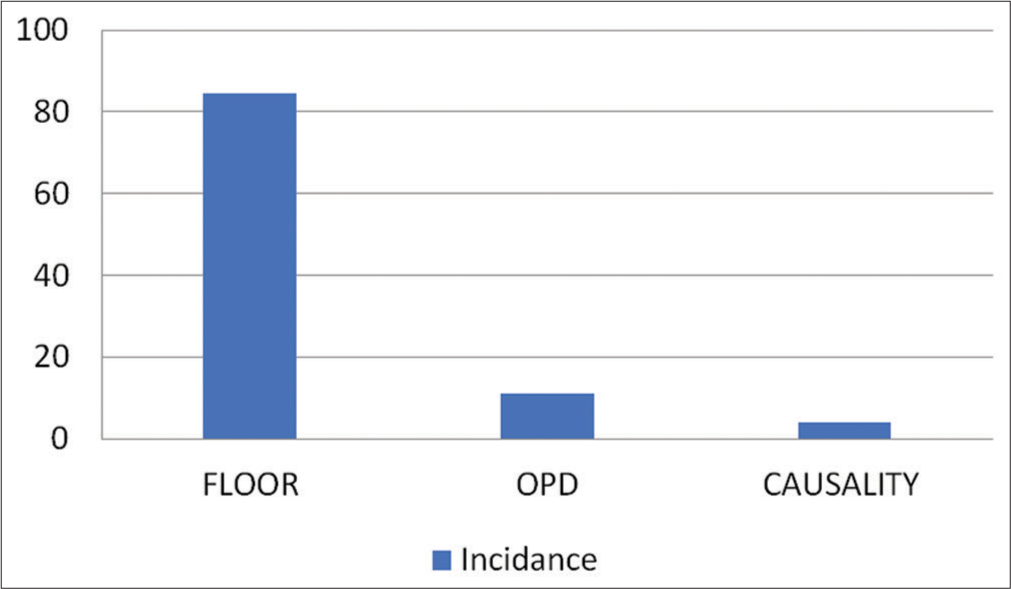
- Incidence rate by departments.

- The extent of the fungal infections during the years from 2009 to 2018 in relation with the source of collection either floor, OPD, or casualty.
The incidence of fungal keratitis has been gradually increasing in the years after 2009, especially after the year of 2013.
DISCUSSION
The patterns and consequences of fungal keratitis at Tripoli Eye Hospital were reported in this study. Much focus has been put on the recent outbreak of fungal keratitis in soft contact lens wearers and the possible reasons for it.[15] The key conclusion of the present study is that the occurrence of fungal keratitis gradually increased in the years after 2009, especially after 2013. In contrast to the common perception of a low frequency of fungal keratitis in the North African region, a high incidence of fungal keratitis among infectious keratitis patients (32.9%) was found in our sample. The Aspergillus and Fusarium genera have caused much of the fungal infections. In North Africa, the higher cases of fungal keratitis can be due to a growing trend toward farming activity in this area that predisposes individuals to vegetative injury. As per the prevalent sociocultural system, males primarily go for outdoor work and the same applies to agriculture, hence the predominance of males in fungal keratitis.
One of the highest crucial causes for infectious keratitis, along with ocular and systemic diseases, is contact lens use. In previous research, contact lens-related microbial keratitis had a high incidence rate.[16] The number of wearers of contact lenses has been growing, and younger people are equipped with contact lenses and do not follow guidelines for appropriate contact lens treatment. The age mode importance of patients in this presentation study was 24 years of age.[17] In addition, orthokeratology has resulted in several people wearing contact lenses overnight.[18]
The use of drugs, particularly steroid eye drops, lowers the immune system and reduces the host defense mechanism. For various ocular disorders such as blepharitis, iridocyclitis, choroiditis, and even allergic conjunctivitis, steroids are typically administered. When unmonitored, the use of steroids for a spectrum of ocular disorders leads to fungal keratitis. Diabetes mellitus has also been identified as a predisposing factor in some patients.[3]
Often, fungal keratitis has worse clinical results than bacterial keratitis. Studies have highlighted the advantage of topical natamycin for fungal keratitis over topical voriconazole, especially among those caused by Fusarium. In addition, voriconazole did not improve overall performance, although among Fusarium ulcers, there may have been some consequence. The authors concluded that they were unable to prescribe oral voriconazole at this time, considering the rise in non-serious adverse effects.[19]
CONCLUSION
In conclusion, fungal keratitis is the leading cause of morbidity in the eye. Popular worldwide risk factors include diabetes mellitus, the use of contact lenses, and corticosteroids, but the most common identifiable cause is traumatic vegetative eye injury. There is significant variation between infectious keratitis because of its varied clinical appearance, and it has a clinical diagnostic challenge. Awareness of common cause clinical cases, related risk factors, and presentations of complications will also aid in the early diagnosis of fungal keratitis and improved clinical outcomes.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The persistent dilemma of microbial keratitis: Global burden, diagnosis, and antimicrobial resistance. Surv Ophthalmol. 2019;64:255-71.
- [CrossRef] [PubMed] [Google Scholar]
- Experimental models for fungal keratitis: An overview of principles and protocols. Cells. 2020;9:1713.
- [CrossRef] [PubMed] [Google Scholar]
- A study of fungal keratitis in North Africa: Exploring risk factors and microbiological features. Int J Life Sci Sci Res. 2016;2:579-82.
- [CrossRef] [Google Scholar]
- Perfil das ceratitesfúngicas no hospital são geraldo belo horizonte-MG. Arq Bras Oftalmol. 2002;65:9-13.
- [CrossRef] [Google Scholar]
- Ocular mycosis at a referral center in Saudi Arabia: A 20-year study. Saudi J Ophthalmol. 2011;25:231-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic information profiling and evaluation of causative fungi of fungal keratitis using high-throughput internal transcribed spacer sequencing. Sci Rep. 2020;10:1640.
- [CrossRef] [PubMed] [Google Scholar]
- Filamentous fungal keratitis in Taiwan: Based on molecular diagnosis. Transl Vis Sci Technol. 2020;9:32.
- [CrossRef] [PubMed] [Google Scholar]
- Local activation of the alternative pathway of complement system in mycotic keratitis patient tear. Front Cell Infect Microbiol. 2020;10:205.
- [CrossRef] [PubMed] [Google Scholar]
- Mycotic keratitis in India: A five-year retrospective study. J Infect Dev Ctries. 2010;4:171-4.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical review of microbial corneal ulcers resulting in enucleation and evisceration in a tertiary eye care center in Hungary. J Ophthalmol. 2020;2020:8283131.
- [CrossRef] [PubMed] [Google Scholar]
- The epidemiological features and laboratory results of fungal keratitis: A 10-year review at a referral eye care center in South India. Cornea. 2002;21:555-9.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors and clinical outcomes of bacterial and fungal scleritis at a tertiary eye care hospital. Middle East Afr J Ophthalmol. 2015;22:203-11.
- [CrossRef] [PubMed] [Google Scholar]
- Fungal keratitis in North India; Spectrum and diagnosis by Calcofluor white stain. Indian J Med Microbiol. 2015;33:462-3.
- [CrossRef] [PubMed] [Google Scholar]
- Pharmacotherapy of fungal eye infections. Expert Opin Pharmacother. 2001;2:1849-57.
- [CrossRef] [PubMed] [Google Scholar]
- Voriconazole in the management of Alternaria keratitis. Cornea. 2006;25:242-4.
- [CrossRef] [PubMed] [Google Scholar]
- In vitro pharmacodynamics of amphotericin B, itraconazole, and voriconazole against Aspergillus, Fusarium, and Scedosporium spp. Antimicrob Agents Chemother. 2005;49:945-51.
- [CrossRef] [PubMed] [Google Scholar]
- In vitro investigation of voriconazole susceptibility for keratitis and endophthalmitis fungal pathogens. Am J Ophthalmol. 2004;137:820-5.
- [CrossRef] [PubMed] [Google Scholar]
- Update on the management of infectious keratitis. Ophthalmology. 2017;124:1678-89.
- [CrossRef] [PubMed] [Google Scholar]







