Translate this page into:
Unilateral proptosis in a 3-year-old child – A case report
*Corresponding author: Rajwinder Kaur,Department of Ophthalmology, Adesh Institute of Medical Sciences and Research, Bathinda, Punjab, India.rajujerry26@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kaur R, Samria S, Singh H. Unilateral proptosis in a 3-year-old child – A case report. Adesh Univ J Med Sci Res 2020;2(2):109-11.
Abstract
Optic nerve gliomas (ONGs) are now regarded as true neoplasm with the ability to invade locally, but are relatively rare. Gliomas arise from astrocytes of the optic nerve and visual pathway. We describe a case of a 3-year-old bo y with painless progressive protrusion left eye for 1 month. The child was evaluated clinically and required investigations were carried out, the findings were consistent with the diagnosis of ONG. Magnetic resonance imaging is diagnostic to see its extension and to plan its management. An integrated approach should involve neuro-ophthalmologists, hemato-oncologist, oculoplastic surgeons, neurosurgeons, and radiation oncologists.
Keywords
Optic nerve glioma
Intracranial tumor
Neurofibromatosis
proptosis
INTRODUCTION
Optic pathway gliomas (OPGs) are low-grade neoplasms arising from the precortical optic pathways. OPG can involve the optic nerve, optic chiasma, optic tracts, optic radiations, or the hypothalamus.[1] Optic nerve gliomas (ONGs) account for half of all primary optic nerve tumors, make between 1.5 and 4% of all orbital tumors 71% of all patients are found in the first decade.[1] They can be divided into three clinical pathological types: Anterior which is confined to the optic disc and optic nerve (25%), chiasmal lesions (20–40%), and posterior lesions involving the hypothalamus with possible extension to the optic tracts (33–60%). The most common histotype entity is low-grade astrocytoma.[2,3] Approximately 15%–20% of patients with type 1 neurofibromatosis (NF 1) eventually develop an OPG.[1] The characteristic of ONG is indolent growth with alternating periods of inactivity and growth with rare cases of spontaneous tumor regression. It usually occurs in the extraocular region of the optic nerve.[4] Symptoms and signs of ONG include proptosis (94%), decreased visual function (88%), nystagmus (24%), optic disc swelling (35%) or disc pallor (59%), hypothalamic signs (26%), and increased intracranial pressure (27%).[1] With the use of high-resolution computerized tomography and magnetic resonance imaging (MRI) scan, the diagnosis of OPG no longer requires biopsy in most cases.[2] Treatment of optic gliomas should be tailored to the individual patient; no clear therapeutic protocol is available.[3] We report a rare case of 3-year-old male child with an ONG who presented with unilateral proptosis.
CASE HISTORY
This is a case report of a 3-year-old male child who presented to our department with chief complaint of painless progressive protrusion of the left eye for 1 month. There was no history of nausea, vomiting, seizures, and ocular trauma. There was no history of NF 1 in the family. There were neither café au lait spots on the patient’s body, nor axillary or inguinal freckling were present.
The child underwent detailed, comprehensive ocular examination and pediatric consultation was also done. Visual acuity in the right eye was 20/20 and 20/400 with the left eye with pediatric picture chart. The right eye examination was within normal limits. The left eye examination revealed axial proptosis of 4–5 mm as measured with Hertel’s exophthalmometer with upper sclera show and inferior dystopia [Figure 1]. There was no history of diplopia and lagophthalmos. Pupil was showing relative afferent pupillary defect (RAPD) in the left eye and there was no apparent squint and nystagmus. Slit lamp biomicroscopy was done which revealed normal iris pattern but no Lisch nodules were seen. The right eye fundus was normal with slightly tilted disc and the left eye fundus showed extensive disc edema and adjacent retinal nerve fiber layer edema, but there were no obvious choroidal folds [Figure 2]. Urgent MRI brain and orbit was done after sedation being advised by pediatric consultation. It confirmed the presence of ONG. Axial MRI T1WI showed well-defined homogenously enhancing fusiform mass involving intraorbital segment of the left optic nerve extending from the level of optic disc causing proptosis of the left eyeball with no extension into the optic canal. The mass measured 2.1 cm × 1.5 cm × 1.7 cm (AP × T × CC). Flattening of posterior aspect of eyeball was seen with subtle edema in the region of optic disc. Optic chiasma was normal. Extra-axial spaces and extraocular muscles of the left eye were normal [Figure 3]. MRI brain and orbit (coronal section) showed homogeneously enhancing mass in left eye which confirmed optic nerve glioma [Figure 4]. The child was then referred to neurosurgery department for further management. They advised radiotherapy to the patient.
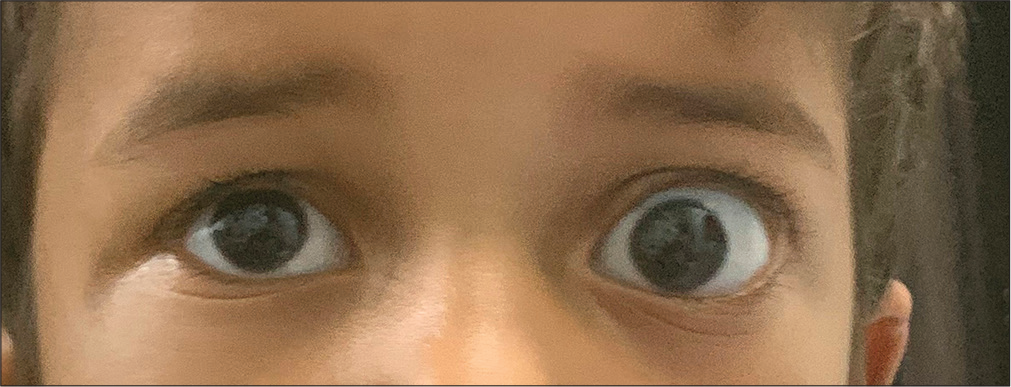
- Axial proptosis and dystopia with scleral show in the left eye.
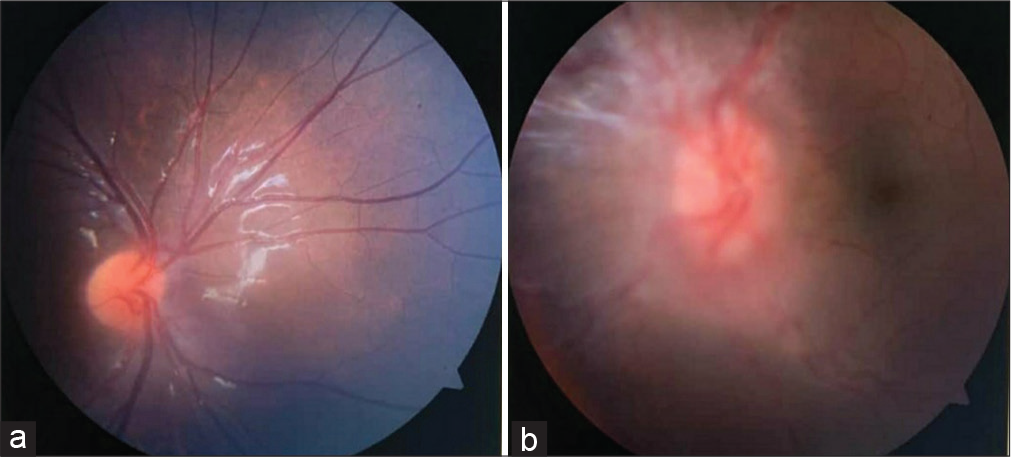
- (a and b) Fundus of the right eye showed slightly tilted disc. The left eye showed extensive disc edema and adjacent retinal nerve fiber layer edema.
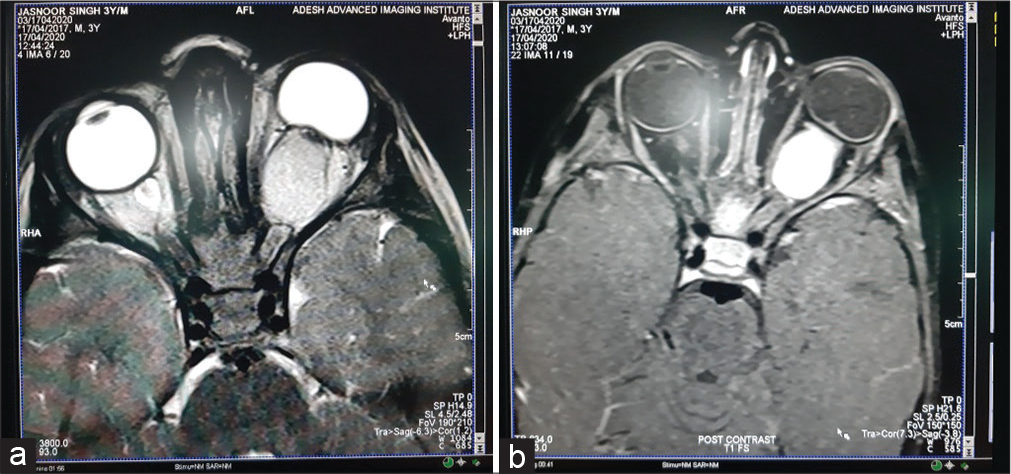
- (a and b) Magnetic resonance imaging brain and orbit showed well-defined homogenously enhancing fusiform mass involving intraorbital segment of the left optic nerve extending from the level of optic disc causing proptosis of the left eyeball with no extension into the optic canal. The mass measured 2.1 cm × 1.5 cm × 1.7 cm (AP × T × CC). Flattening of posterior aspect of eyeball was seen with subtle edema in the region of optic disc. Optic canal and optic chiasm were normal. Extra-axial spaces and extraocular muscles of the left eye were normal

- Magnetic resonance imaging of brain and orbit (coronal section) showed homogeneously enhancing mass in the left eye.
DISCUSSION
ONGs are slow-growing tumors which usually affect children under age of 20 years.[3] The differential diagnosis of child with proptosis, RAPD, and painless loss of vision included ONG, optic neuritis, optic nerve meningioma, and autosomal dominant optic atrophy.[1] Because of their central location and either through direct extension through optic canal or mass effect, ONGs account for endocrine abnormalities and neurological complications. Enlargement of the optic canal is seen in 80% of patients where the optic nerve is involved.[5] Both ONG and meningioma can show diffuse globular or fusiform enlargement of the optic nerve. However, meningioma shows “tram-track” sign and calcification in 20–30% of cases.[1]
In this case report, the patient presented with unilateral proptosis which is a typical feature of ONGs in association with proptosis and disc edema, as shown by Ghazal et al.,[2] Mehta et al.,[5] Gupta et al.,[6] and many others. In our case, the time of presentation was 3 years which is consistent with other studies done by Mehta et al.[5] and Gupta et al.[6] NF-1 has been observed in approximately 25% of cases unlike our case where there are no signs of NF-1 at present.[4] The remarkable feature of our case is the presence of disc edema with proptosis at very early age which is a poor prognostic factor. Optic nerve glioma is rare in occurance. Vision threatening as well as life threatening complications are known to occur which makes the early diagnosis and its appropriate management to be mandatory. NF-1 associated OPG is generally considered to have a better prognosis.
Various modalities of management are available ranging from a conservative approach to a combination of radiotherapy, chemotherapy, and surgical removal.[3] The complexity of the disease requires individualized specific interventional strategies.[1,2] Management is tailored depending on various factors including patient age, vision and vision change, symptoms, NFL status, clinical course, nature and progression of the tumor, neoplasm genetics, and patient preference. Observation is the first choice until significant visual deficits or there is progression radiologically. More recently, it has been shown that stabilization of vision and more limited progression of the tumor may be achieved with radiotherapy. Surgery should be limited when there are excessive proptosis and pain or when they extend posterior. The risk of loss of vision is substantial, when surgery is performed when vision is present. Chemotherapy is considered in most cases, but has an increased risk of secondary leukemia and should, therefore, be avoided.[1]
CONCLUSION
ONGs pose a great challenge to the ophthalmologists due to wide variety of presentation, vision assessment, and its management in very young children. Management of ONGs is a multidisciplinary approach. Counseling of the parents is again a bigger challenge, especially while educating them about loss of vision in the involved eye.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Optic nerve glioma In: Stat Pearls. Treasure Island, FL: Stat Pearls Publishing; 2020.
- [Google Scholar]
- Radiation therapy in optic gliomas: A case report and a review of literature. J Nucl Med Radiat Ther. 2012;3:134.
- [Google Scholar]
- Optic nerve glioma with complete intraocular extension. J Curr Ophthalmol. 2016;28:228-31.
- [CrossRef] [PubMed] [Google Scholar]
- Optic nerve glioma with unilateral proptosis: An interesting case report. IJSS Case Rep Rev. 2014;1:1-2.
- [Google Scholar]
- Rare case of optic pathway glioma with extensive intraocular involvement in a child with neurofibromatosis type 1. Middle East Afr J Ophthalmol. 2015;22:117-8.
- [CrossRef] [PubMed] [Google Scholar]







